
Pregnancy Medication Safety Checker
When you’re pregnant, every pill, drop, or patch feels like a gamble. You take something to ease a headache, manage nausea, or control a chronic condition-and suddenly, you’re wondering: could this hurt my baby? The fear isn’t irrational. Around 2-3% of birth defects are linked to medications taken during pregnancy. That number might sound small, but for the families affected, it’s everything.
What Exactly Is a Teratogen?
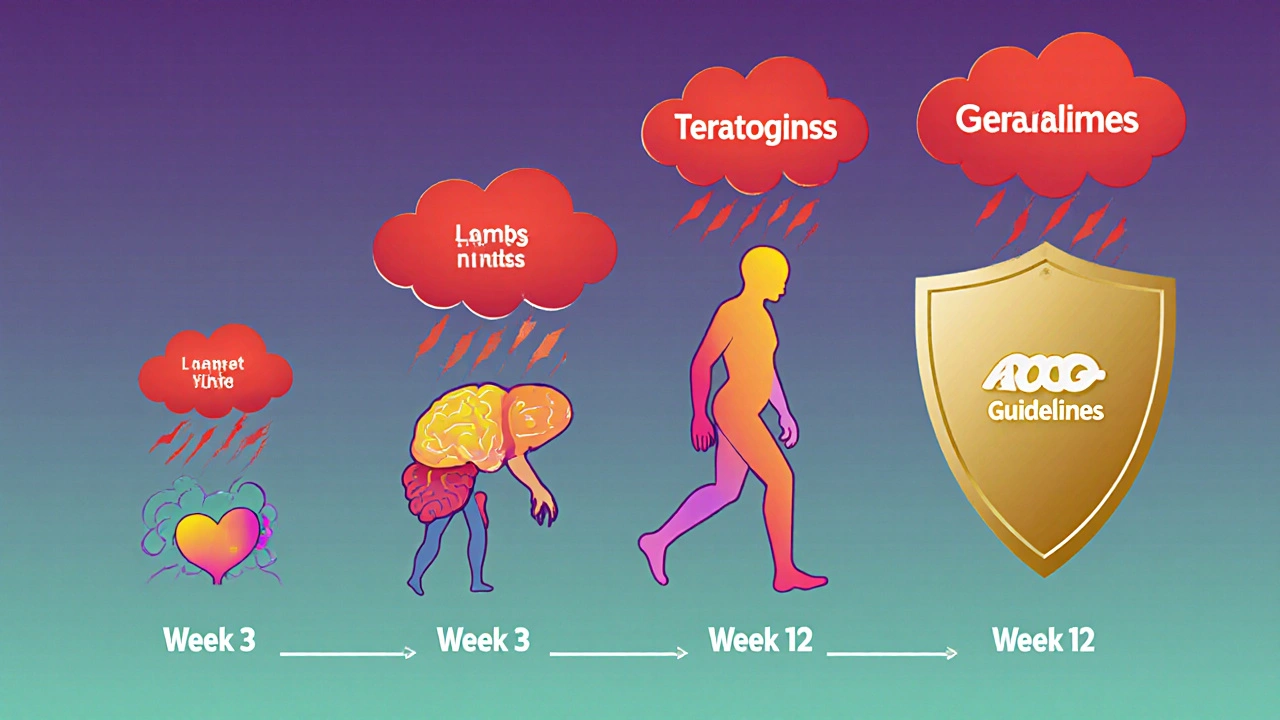
A teratogen is any substance-medication, chemical, infection, or even radiation-that can interfere with fetal development and cause birth defects. Not all drugs are teratogens. In fact, most medications you take during pregnancy don’t cause harm. But some do, and the risk isn’t the same at every stage.The first trimester is the most sensitive window. Between weeks 3 and 8 after conception, your baby’s organs are forming. That’s when exposure to certain drugs can lead to major structural problems-like missing limbs, heart defects, or neural tube defects. After week 12, the risk shifts. Instead of changing the shape of organs, drugs might affect how they function-leading to issues like low birth weight, developmental delays, or withdrawal symptoms after birth.
Medications with Proven Risks
Some drugs are known dangers during pregnancy. These aren’t hypothetical risks-they’re backed by decades of data.- Warfarin (a blood thinner): Can cause fetal warfarin syndrome, which includes underdeveloped noses, bone problems, eye damage, and intellectual disabilities. The risk is highest in the first trimester.
- Methotrexate (used for cancer, autoimmune diseases): A folate blocker that increases neural tube defect risk by 10-20%. It’s absolutely not safe in early pregnancy.
- Carbamazepine (for epilepsy): Carries a 1% risk of spina bifida and can cause bleeding in newborns due to vitamin K deficiency.
- Factor Xa inhibitors (rivaroxaban, apixaban): These newer blood thinners cross the placenta. There’s no antidote if bleeding happens, and human safety data is extremely limited.
- Cannabis (THC): Linked to a 15-20% higher chance of low birth weight, 10-15% higher risk of preterm birth, and possible long-term effects like attention problems and lower IQ scores. THC stays in breastmilk for up to six days after use.
These aren’t rare cases. They’re well-documented outcomes. If you’re on any of these medications and planning pregnancy-or already pregnant-talk to your doctor immediately. Don’t stop cold turkey, but don’t wait either. A safe alternative often exists.
The Acetaminophen Debate
No drug has sparked more confusion than acetaminophen (paracetamol). It’s in Tylenol, Excedrin, and countless cold remedies. For years, it was the go-to pain reliever for pregnant women because it was considered safe.Now, things are messy. Some studies suggest a link between long-term acetaminophen use and higher risks of ADHD or autism in children. The CDC mentions this as a potential concern. But here’s the other side: the American College of Obstetricians and Gynecologists (ACOG) issued a clear statement in September 2025 saying not treating fever or pain is far more dangerous.
Why? Because untreated fever during early pregnancy increases the risk of neural tube defects by 20-30%. Uncontrolled pain can raise stress hormones, which may affect fetal development too. ACOG’s position is simple: if you need acetaminophen, use it. The benefits outweigh the unproven risks.
This isn’t a contradiction-it’s context. One study doesn’t prove causation. But a mother’s untreated illness can be deadly. The key is using the lowest effective dose for the shortest time. Don’t take it daily for weeks without a reason. But don’t suffer through migraines or fevers either.
How Pregnancy Risk Labels Changed
You might remember the old A, B, C, D, X labels on medicine bottles. Those are gone. In 2015, the FDA replaced them with the Pregnancy and Lactation Labeling Rule (PLLR). Now, drug labels include detailed sections: risks, clinical considerations, and data sources.Why the change? Because “Category D” didn’t tell you if the risk was 1% or 30%. It didn’t say whether the danger was in week 5 or week 25. The new labels give you real information: “In animal studies, this drug caused heart defects at high doses. In 200 human pregnancies, no birth defects were reported.”
But here’s the catch: about 70-80% of medications still lack solid data on pregnancy safety. That’s because testing drugs on pregnant women is ethically impossible. Most of what we know comes from accidental exposures, case reports, or animal studies. So even if a drug doesn’t have a clear warning, it doesn’t mean it’s proven safe.
What You Should Do Before and During Pregnancy
You don’t have to guess. There’s a system to help you.- Before you get pregnant: Review every medication you take-prescription, over-the-counter, supplements, herbs-with your doctor or pharmacist. Some medications need to be switched months in advance. For example, if you’re on isotretinoin (Accutane) for acne, you must stop at least one month before trying to conceive.
- When you’re pregnant: Never start a new medication without checking with your provider. Even “natural” remedies like St. John’s Wort or high-dose vitamin A can be risky.
- For chronic conditions: Don’t stop your meds because you’re scared. If you have epilepsy, high blood pressure, or depression, stopping your treatment can be more dangerous than the drug itself. Your doctor can often switch you to a safer version.
- Use trusted resources: MotherToBaby (a service run by teratology experts) offers free, science-based advice. LactMed (from the NIH) tells you about drugs and breastfeeding. Don’t rely on Google or Reddit.
More than 90% of pregnant women take at least one medication. That’s normal. The goal isn’t to be drug-free-it’s to be informed. The right medication, at the right time, can save your life and your baby’s.

Why Confusion Is So Common
You’re not alone if you feel lost. One Reddit user wrote: “My OB said Zofran was fine for morning sickness. Then I read online it might cause birth defects. I cried for days.”That’s the problem. Online forums mix truth with fear. A single case report gets turned into a headline. A 2018 mouse study becomes “Proven to cause autism.” Meanwhile, experts at MotherToBaby handle over 10,000 calls a year-mostly about acetaminophen, antidepressants, and anti-nausea drugs. The top concern? Contradictory advice.
Here’s the reality: science moves slowly. What we know today might change tomorrow. But that doesn’t mean you should panic. It means you need a guide. Your OB, your pharmacist, your midwife-they’re your team. Use them.
What’s Next for Pregnancy Medication Safety
The future is getting better. The FDA’s Sentinel Initiative is tracking 10 million patient records to find patterns in real-world use. Researchers are starting to use genetic testing to predict who might be more sensitive to certain drugs. Within five years, we may be able to say: “Based on your genes, this medication is low-risk for you.”But right now, the biggest barrier isn’t science-it’s funding. Less than 3% of maternal health research money goes to studying medications. That’s why so many drugs are still in the “unknown” zone.
For now, the best tools you have are awareness and communication. Know what you’re taking. Ask why. Ask about alternatives. Ask what happens if you don’t take it.
You’re not just protecting your baby. You’re protecting yourself. And that’s the most important thing of all.
Can I take ibuprofen while pregnant?
Avoid ibuprofen after 20 weeks of pregnancy. It can cause low amniotic fluid and kidney problems in the baby. Before 20 weeks, occasional use is usually okay, but acetaminophen is still the safer choice. Always check with your provider first.
What if I took a medication before I knew I was pregnant?
Don’t panic. Most medications don’t cause harm, and many exposures happen before a woman even knows she’s pregnant. The critical period for major birth defects is between weeks 3 and 8. If you took something before then, the risk is often very low. Call MotherToBaby or your doctor-they can assess your specific situation based on the drug, dose, and timing.
Are antidepressants safe during pregnancy?
Some antidepressants, like sertraline and citalopram, are considered low-risk during pregnancy. Untreated depression, however, increases risks of preterm birth, low birth weight, and postpartum complications. The decision isn’t about whether the drug is perfect-it’s about whether stopping it is worse. Work with your psychiatrist and OB to find the safest option.
Is it safe to use topical medications during pregnancy?
Most topical creams, ointments, and patches have very little absorption into the bloodstream, so they’re usually low risk. But avoid strong retinoids (like tretinoin) or high-dose salicylates. Always check with your provider-even if it’s just a cream for eczema.
Can I rely on online pregnancy drug safety apps?
Some apps are helpful, but many are outdated or based on opinion, not science. Stick to trusted sources like the FDA’s label info, MotherToBaby, or LactMed. If an app says a drug is “100% safe,” it’s likely wrong. No drug is 100% risk-free in pregnancy. The goal is informed risk management, not false certainty.
What to Do Next
If you’re planning pregnancy: schedule a medication review with your doctor or pharmacist. Bring a list of everything you take-even vitamins and herbal teas.If you’re already pregnant: don’t stop or start anything without talking to your provider. Keep a log of every medication you use, including when and why.
If you’re unsure: call MotherToBaby at 1-866-626-6847. They’re free, confidential, and staffed by specialists who know exactly what you’re going through.
You don’t have to navigate this alone. The right information, at the right time, makes all the difference.




Jessica Glass
October 29, 2025 AT 18:05Oh wow, another ‘trust your doctor’ pep talk. Because clearly, OBs are just angels in scrubs who never make mistakes. I’ve seen three friends miscarry after being told ‘it’s fine’ by their ‘trusted’ providers. The system is broken, and no amount of FDA jargon fixes that. You’re not protecting your baby-you’re trusting a profit-driven machine that doesn’t even track long-term neurodevelopmental outcomes.
And don’t get me started on ‘MotherToBaby.’ It’s funded by pharma. Of course they say acetaminophen is fine. They’d say the same thing about thalidomide if it had a patent.
Stop gaslighting pregnant people. We’re not paranoid. We’re just tired of being lab rats with belly buttons.
Krishna Kranthi
October 30, 2025 AT 11:09Bro in India here and let me tell you-our grandmas would’ve laughed at this whole debate
Back in the day we took neem leaves for fever turmeric for everything and nobody knew what a teratogen was
But somehow we had healthy babies
Now we got apps and labels and PhDs arguing over Tylenol like it’s the Holy Grail
Maybe the answer isn’t more data but less fear
Also THC in breastmilk for six days? Bro I’ve seen moms smoke while nursing and their kids are now IIT engineers
Science is cool but don’t forget culture
Also I love this post so much I cried a little
Not because I’m scared
But because someone finally said it without the corporate tone
Lilly Dillon
October 31, 2025 AT 10:34I took acetaminophen for three weeks during my first trimester because I had a sinus infection and couldn’t sleep. I didn’t panic. I didn’t Google. I just called my midwife and she said, ‘You’re fine.’
My son is now seven, plays piano, and has perfect vision.
Don’t let fear turn your pregnancy into a minefield. Trust your provider. Trust your body. Trust that you’re not the first person to take a pill while pregnant.
And if you’re still anxious? Breathe.
Shiv Sivaguru
October 31, 2025 AT 15:07So let me get this straight-10k calls a year to MotherToBaby and 90% are about Tylenol and SSRIs
That’s not a public health crisis
That’s a marketing crisis
Pharma spends billions making moms feel guilty so they’ll buy ‘safe’ alternatives that cost 5x more
And now we’ve got Reddit threads where women cry over ibuprofen like it’s a death sentence
Meanwhile the real killers are air pollution and food deserts
But nah let’s just panic about a $2 pill
Capitalism wins again
Gavin McMurdo
November 1, 2025 AT 03:26Let’s be brutally honest: the entire pregnancy medication landscape is a performance. The FDA’s new labeling system? A PR stunt. The ‘clinical considerations’ section? A legal loophole dressed in jargon.
They don’t give you data-they give you narratives. ‘In 200 human pregnancies, no birth defects were reported.’ That’s not science. That’s a sentence written by a lawyer who doesn’t want to get sued.
And don’t even get me started on ‘natural remedies.’ St. John’s Wort is dangerous? Tell that to the 19th-century midwives who used it to induce labor.
There’s no such thing as ‘safe.’ There’s only ‘acceptable risk.’ And who decides what’s acceptable? Not you. Not your doctor. The insurance company does.
Stop pretending this is about your baby. It’s about liability.
Jesse Weinberger
November 2, 2025 AT 01:31Acetaminophen causes autism? lol nope
but wait… what if it DOES?
what if the real cause is 5G + glyphosate + fluoride + vaccines + wifi + blue light + GMOs + soy + gluten + dairy + sugar + plastic + air pollution + EMFs + microwaves + processed food + social media + capitalism + patriarchy + the moon phases
you think they’re gonna tell you that?
they want you to take tylenol so you dont scream at your husband
and keep buying their stuff
also i took benadryl for sleep during pregnancy
my kid now thinks he’s a dolphin
coincidence?
i think not
Emilie Bronsard
November 3, 2025 AT 22:42I appreciate how balanced this is. It’s easy to fall into fear, but the real danger is doing nothing. I had preeclampsia and was on low-dose aspirin. I was terrified. But my OB showed me the data-my risk of complications dropped by 60%.
It’s not about avoiding all risk. It’s about choosing the least harmful path.
Thank you for saying that clearly.
John Bob
November 5, 2025 AT 05:27They say ‘don’t stop your meds.’ But what if your meds are part of the problem? What if the depression you’re treating was caused by the same pharmaceutical industry that now tells you it’s safe to keep taking them?
Have you ever read the full FDA adverse event reports for SSRIs in pregnancy? The ones they don’t put in the ‘clinical considerations’ section?
There’s a reason why Scandinavian countries have lower rates of antidepressant use during pregnancy-and lower rates of autism.
Coincidence?
Or is this just another case of American medical exceptionalism?
Don’t trust the system. Question everything.
Alex Grizzell
November 6, 2025 AT 19:36Hey mama-you got this.
I know it feels like every pill is a bomb waiting to go off. But you’re not alone. I was terrified too when I had to take prednisone for my asthma during pregnancy.
I called MotherToBaby. They walked me through the risks. They didn’t scare me. They empowered me.
My daughter is 3 now and runs like a cheetah.
Don’t let fear steal your joy. You’re doing better than you think.
And if you need to cry? Cry. Then call your provider. Then breathe. You’re not failing. You’re fighting.
George Johnson
November 8, 2025 AT 05:25So we’re now treating pregnancy like a chemistry lab where every pill is a potential war crime
Meanwhile my cousin in Kerala took her grandma’s herbal paste for nausea and gave birth to twins who now run a chai stall
Maybe the real teratogen is anxiety
Also why is everyone so scared of THC but fine with 3 cups of coffee and 2 glasses of wine?
Double standard much?
Rodrigo Ferguson
November 8, 2025 AT 05:37It is, indeed, a matter of considerable concern that the contemporary obstetric paradigm, in its zeal for risk mitigation, has devolved into a performative spectacle of pharmacological compliance, wherein maternal agency is systematically subordinated to institutionalized protocols predicated upon incomplete longitudinal data.
The FDA’s PLLR, while ostensibly an improvement, remains a semiotic facade-masking the epistemological vacuum that persists in maternal-fetal pharmacology.
One must ask: if the corpus of evidence is insufficient to establish safety, how can one ethically endorse any intervention?
And yet-we are exhorted to ‘use the lowest effective dose.’
By whom? For whose benefit?
One suspects the answer lies not in fetal well-being, but in liability management.
It is not science. It is jurisprudence in scrubs.
Mickey Murray
November 9, 2025 AT 18:04Let’s be real-most of this is just fear porn wrapped in science. You think a mom who took one ibuprofen at 18 weeks is gonna have a baby with kidney failure? Nah. She’s gonna have a kid who hates broccoli and loves video games.
Meanwhile, the real villains are the junk food companies pushing sugary snacks to pregnant women because ‘it’s okay, you’re eating for two.’
And don’t even get me started on how we treat depression. We’d rather give you a pill than fix your sleep schedule, your partner’s emotional neglect, or your 80-hour workweek.
Stop blaming the meds. Start blaming the system.
And if you’re still stressed? Go for a walk. Drink water. Eat real food. You don’t need a pill for that.
Kevin McAllister
November 11, 2025 AT 02:17THEY’RE LYING TO YOU. EVERY SINGLE ONE OF THEM. The FDA? Corporate puppets. The OBs? Paid by Big Pharma. MotherToBaby? Funded by Johnson & Johnson. Even your ‘trusted’ pharmacist? They get bonuses for pushing certain brands.
Acetaminophen? It’s a slow poison that erodes your child’s dopamine receptors. THC? It’s a neurotoxin. Warfarin? That’s a war crime waiting to happen.
And they want you to believe it’s all ‘just a 1% risk’?
1% of 4 million births is 40,000 babies. That’s a small town. Every year.
Don’t be a sheep. Do your own research. Buy a fetal Doppler. Track your vitals. Eat organic. Avoid ALL plastics. Sleep on copper sheets. And if you take anything? Only what your great-grandma used.
They don’t want you to know the truth.
But now you do.
Marcia Martins
November 12, 2025 AT 21:02I just wanted to say thank you for writing this. I was so scared after my first ultrasound and ended up crying in the parking lot. I didn’t know what to believe.
This post didn’t make me feel guilty. It made me feel informed.
I’m 22 weeks now. I take my prenatal vitamins, my iron, and my occasional Tylenol for headaches.
I’m not perfect.
But I’m trying.
And that’s enough.
Robert Bowser
November 13, 2025 AT 04:25My wife took a single dose of ibuprofen at 19 weeks because she had a migraine. We called MotherToBaby the next day. They said, ‘One dose? No concern.’
Our daughter is 2 now. She’s healthy, smart, and loves bananas.
Don’t let fear turn pregnancy into a prison.
Be informed. Be cautious. But don’t be paralyzed.
You’re not alone.
Jessica Glass
November 13, 2025 AT 12:14So now we’re supposed to trust the same system that told us thalidomide was safe? That told us DES was fine? That told us cigarettes were okay for pregnant women?
History doesn’t repeat, but it rhymes.
And right now, the rhyme is acetaminophen.
They said the same thing about that in the 90s.
And now we’re seeing a 30% spike in ADHD diagnoses.
Coincidence?
Or just the next chapter in the same damn book?