
Side Effect Visibility Calculator
See how clinical trial size affects side effect detection. Input your trial size and side effect frequency to understand why some side effects only appear after a drug is widely used.
When you take a new medication, you’re trusting that it’s safe. The label lists possible side effects, but those numbers? They don’t tell the whole story. Clinical trial data and real-world side effect data are two different worlds - and understanding the gap between them could literally save your life.
What Clinical Trials Actually Show
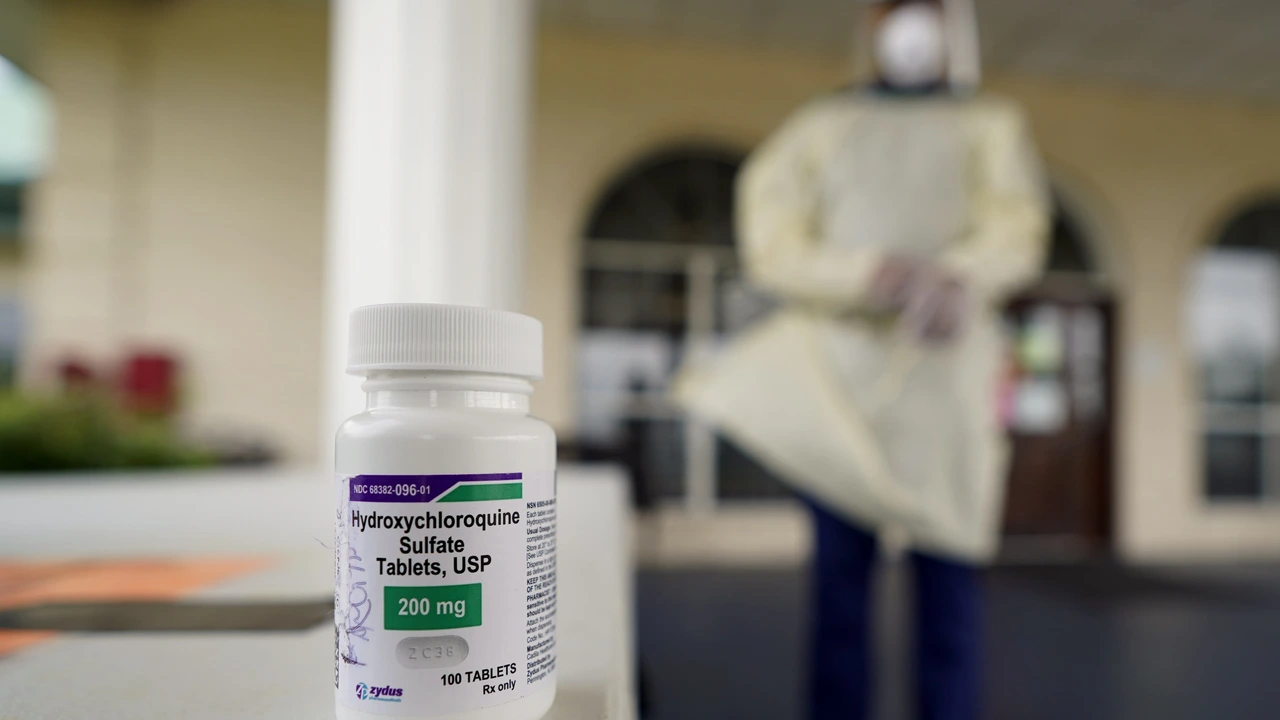
Clinical trials are designed to answer one question: does this drug work under perfect conditions? They’re tightly controlled. Participants are carefully selected - usually healthy adults, no major other illnesses, no other medications that might interfere. They’re monitored closely, with check-ins every week or month. Side effects are recorded using a standardized system called CTCAE v5.0, which has 790 specific terms for everything from mild nausea to death. But here’s the catch: these trials are small. The average Phase 3 trial for cancer drugs includes just 381 people. That means if a side effect happens in 1 in 500 people, it’s unlikely to show up at all. Rosiglitazone, a diabetes drug approved in 1999, didn’t show a clear heart risk in trials. But after millions of people started taking it, real-world data revealed a 43% higher risk of heart attacks. That risk was invisible in the trial. Clinical trials are great at spotting common, serious side effects - like liver damage or severe allergic reactions - because they’re designed to catch the big red flags. But they’re blind to rare, delayed, or subtle effects. They also don’t reflect how real people live. No trial includes someone working two jobs, forgetting doses, or taking herbal supplements because they “feel better.”What Real-World Data Reveals
Real-world data comes from everywhere: hospitals, pharmacies, insurance claims, patient apps, and even social media. The FDA’s Adverse Event Reporting System (FAERS) got over 2.1 million reports in 2022. That’s up from 1.4 million in 2018. These aren’t controlled studies. They’re spontaneous reports - doctors, pharmacists, or patients noticing something odd and filing a note. This is where the hidden dangers show up. Take fluoroquinolone antibiotics. Clinical trials didn’t flag serious nerve and tendon damage. But real-world analysis of 1.2 million patient records led the European Medicines Agency to restrict their use in 2019. Same with pioglitazone - the heart failure risk wasn’t clear until 10 years of real-world data tracked over 190,000 patients. Real-world data also catches things trials miss because of lifestyle. A 2022 survey found 63% of patients experienced side effects not listed on their drug’s FDA label. Nearly half of those were moderate to severe - fatigue, brain fog, dizziness - symptoms that didn’t show up in trials because patients weren’t asked about them outside clinic visits. Patients using apps like MyTherapy reported 27% more fatigue with immunotherapy drugs than clinical trials did. Why? Because in trials, fatigue was only recorded during office visits. At home, in the evening, after work, after kids’ bedtime - that’s when it hit hardest. No one asked.Why Real-World Data Can Be Misleading
Real-world data isn’t perfect. It’s messy. Only 2% to 5% of actual side effects ever get reported to FAERS. Most doctors don’t report them - a 2021 AMA survey found only 12% of physicians consistently file reports. It takes 22 minutes per case. Who has time? And then there’s noise. In 2018, a real-world study claimed anticholinergic drugs caused dementia. It turned out the patients already had early signs of dementia - the drugs weren’t the cause. The symptoms came first. The drug was just being taken. That’s called confounding. Real-world data doesn’t control for this. Clinical trials do. EHRs (electronic health records) are another problem. There are over 15 different systems used in U.S. hospitals. One doctor might write “nausea,” another writes “upset stomach,” another doesn’t write anything at all. A 2022 FDA pilot found only 34% of EHR-reported side effects had enough detail to be useful for regulators.How They Work Together
The FDA doesn’t pick one over the other anymore. It uses both. In 2022, 67% of new drug approvals included real-world evidence in post-marketing safety plans. That’s up from 29% in 2017. The 21st Century Cures Act of 2016 made this shift official. Think of it like a two-step safety net. Clinical trials catch the obvious, serious risks before a drug hits the market. Real-world data catches what slips through - the rare reactions, the long-term effects, the interactions with other meds or lifestyle habits. The FDA’s Sentinel Initiative now monitors 300 million patient records in near real-time. It uses 17 different analytical methods to spot patterns. If 10,000 people on a new drug suddenly start having the same rare symptom, Sentinel flags it. Then, experts dig in. Is it real? Or just coincidence? Apple’s Heart Study, with 419,093 participants, proved that mobile tech can capture real-world data at trial scale. Google Health’s AI analyzed 216 million clinical notes and found 23% more drug-side effect links than traditional methods. But here’s the bottom line: real-world data doesn’t replace clinical trials. It complements them. Clinical trials tell you what works under ideal conditions. Real-world data tells you what happens when you let millions of people use it.
What This Means for You
If you’re prescribed a new drug, the label isn’t the full story. Side effects listed there are the ones seen in trials - the common ones, the serious ones. But what about the fatigue you feel every night? The brain fog that makes you forget your keys? The dizziness when you stand up? Those might not be on the label. Track your own symptoms. Use apps like MyTherapy or even a simple journal. Note when they happen, how bad they are, and what else you’re doing or taking. If something feels off, don’t assume it’s just “in your head.” Talk to your pharmacist. They see real-world patterns every day. One Reddit thread from October 2023 had 147 comments from pharmacists saying GLP-1 agonists (like Ozempic) cause way more GI issues in real life than trials suggested. And if you’re a patient with a rare condition or a chronic illness - you’re not just a statistic. Your experience matters. Real-world data is built from people like you.The Future: Blending Both Worlds
The future of drug safety isn’t clinical trials OR real-world data. It’s both - together. Pharmaceutical companies are now building real-world data collection into late-stage trials. Pfizer, Merck, and others are asking patients to use wearables or apps during trials to capture side effects outside the clinic. That’s called hybrid evidence. The FDA’s 2023 Real-World Evidence Framework requires every new drug application to include a plan for post-marketing real-world monitoring. That’s huge. It means drug companies can’t just hand over trial data and walk away. But here’s the challenge: most doctors aren’t trained to interpret real-world data. A 2023 study found only 38% of physicians could correctly understand it without special training. Only 15% of U.S. medical schools teach real-world evidence at all. So if you’re taking a new medication, don’t wait for your doctor to explain it. Ask: “What side effects were seen in trials? What’s been reported since it came out?” If they don’t know, ask for a pharmacist’s input. Or check the FDA’s website for safety communications. The system isn’t perfect. But it’s getting better. And your awareness - your questions, your tracking, your voice - is the most powerful tool you have.Why aren’t all side effects listed on my drug’s label?
Drug labels only include side effects seen during clinical trials, which involve a limited number of people under controlled conditions. Rare side effects, long-term effects, or those triggered by lifestyle factors (like diet, other meds, or stress) often don’t appear until the drug is used by millions of people in the real world. The FDA updates labels as new evidence emerges - but that can take years.
Can real-world data be trusted if it’s so messy?
Yes - but only when analyzed properly. Real-world data is noisy, incomplete, and full of biases. But agencies like the FDA use advanced tools - like the Sentinel Initiative - to filter out false signals. They look for patterns across millions of records, rule out confounding factors, and validate findings before taking action. It’s not perfect, but it’s the best tool we have for spotting hidden risks after a drug is approved.
Do clinical trials miss serious side effects?
Yes, and often. A 2020 JAMA study found clinical trials miss 78% of serious adverse events that show up in real-world use. Why? Because trials exclude older adults, pregnant women, people with multiple conditions, and those on other medications. Real patients don’t fit the trial mold - and that’s exactly when dangerous side effects emerge.
How long does it take for a real-world side effect to be recognized?
It varies. Sometimes it takes months - like when Twitter detected early signals about ivermectin side effects 47 days before official reports. Other times, it takes years, like with rosiglitazone, where the heart risk wasn’t confirmed until 8 years after approval. The FDA’s Sentinel system can now detect signals 6-12 months faster than old methods, but validation still takes time.
Should I stop taking my medication if I notice a side effect not on the label?
Never stop a prescribed medication without talking to your doctor. Many side effects are mild and temporary. But if you notice something new, persistent, or severe - especially if it affects your daily life - document it and report it. Use your pharmacy’s reporting system, an app like MyTherapy, or ask your doctor to file a report with FAERS. Your report could help others.




Katelyn Sykes
November 18, 2025 AT 00:22Been on a new med for anxiety and honestly the label didn't mention the brain fog that made me forget my own birthday. Real world data? Yeah that's the stuff they don't tell you. I started tracking it in MyTherapy and now my pharmacist remembers my name. That's power right there.
Kristina Williams
November 19, 2025 AT 13:01They're hiding stuff. Big Pharma knows the side effects but they bury them so you keep buying. I saw a doc on YouTube who said the FDA gets paid by drug companies. That's why your label is wrong. They don't want you to know about the nerve damage or the depression that comes later. Watch out.
Shilpi Tiwari
November 20, 2025 AT 23:59The confounding variables in real-world EHRs are non-trivial, especially when dealing with polypharmacy in geriatric populations. The signal-to-noise ratio in FAERS is abysmal without robust propensity score matching or instrumental variable analysis. We need standardized ontologies for adverse event coding across EMR systems to enable meta-analyses at scale.
Christine Eslinger
November 21, 2025 AT 23:10It's not about trusting the system. It's about trusting yourself. The label is a starting point, not the whole story. If something feels off, it probably is. Keep a journal. Talk to your pharmacist. Share your story. You're not just a data point-you're a person with a voice. And that voice? It's changing how drugs are monitored. One report at a time.
Denny Sucipto
November 22, 2025 AT 22:02Man, I had that same fatigue with my immunotherapy. Thought I was just tired from work. Turns out it was the drug. I told my doc, he didn't blink. Said he'd seen it before. That's why you gotta speak up. Your tiredness might be someone else's warning sign. Don't brush it off. Write it down. Tell someone.
Heidi R
November 24, 2025 AT 13:12You're all so naive. They don't care about you. Your journal? Your app? Useless. The system is rigged. They'll never change. Just take your pills and shut up.
Brenda Kuter
November 26, 2025 AT 07:32I KNOW THEY'RE LYING. I had tremors, insomnia, and my hair started falling out. I went to three doctors and they all said it was stress. Then I found a Reddit thread with 500 people with the EXACT same symptoms. That drug should be BANNED. Why won't anyone listen? I'm not crazy. I'm just one of the millions they ignored.
Shaun Barratt
November 27, 2025 AT 09:24While the article presents a compelling argument for integrating real-world evidence into pharmacovigilance frameworks, one must acknowledge the inherent limitations of spontaneous reporting systems. The absence of a control group, selection bias, and temporal ambiguity significantly undermine causal inference. Rigorous observational study designs remain indispensable.
Iska Ede
November 27, 2025 AT 23:13So let me get this straight. You want me to pay $200 for a drug that might give me brain fog, then spend my evenings logging my symptoms in an app so some FDA algorithm can finally notice? Brilliant. Next they'll charge me for the privilege of being a human guinea pig.
Gabriella Jayne Bosticco
November 28, 2025 AT 00:23I've been a pharmacist in London for 18 years. The gap between trial data and real life? It's wider than people think. We see the same patterns over and over-fatigue, dizziness, GI issues that don't make the label. Patients don't report them because they think it's normal. But it's not. Your experience matters. Keep talking.
Sarah Frey
November 29, 2025 AT 11:29The convergence of clinical trial rigor and real-world evidence represents a paradigm shift in post-marketing surveillance. The FDA’s Sentinel Initiative exemplifies a scalable, data-driven approach to pharmacovigilance that harmonizes statistical validity with population-level relevance. Continued investment in interoperable health data infrastructure is paramount to sustaining this evolution.