
Medication Interaction Checker
Check for Dangerous Interaction
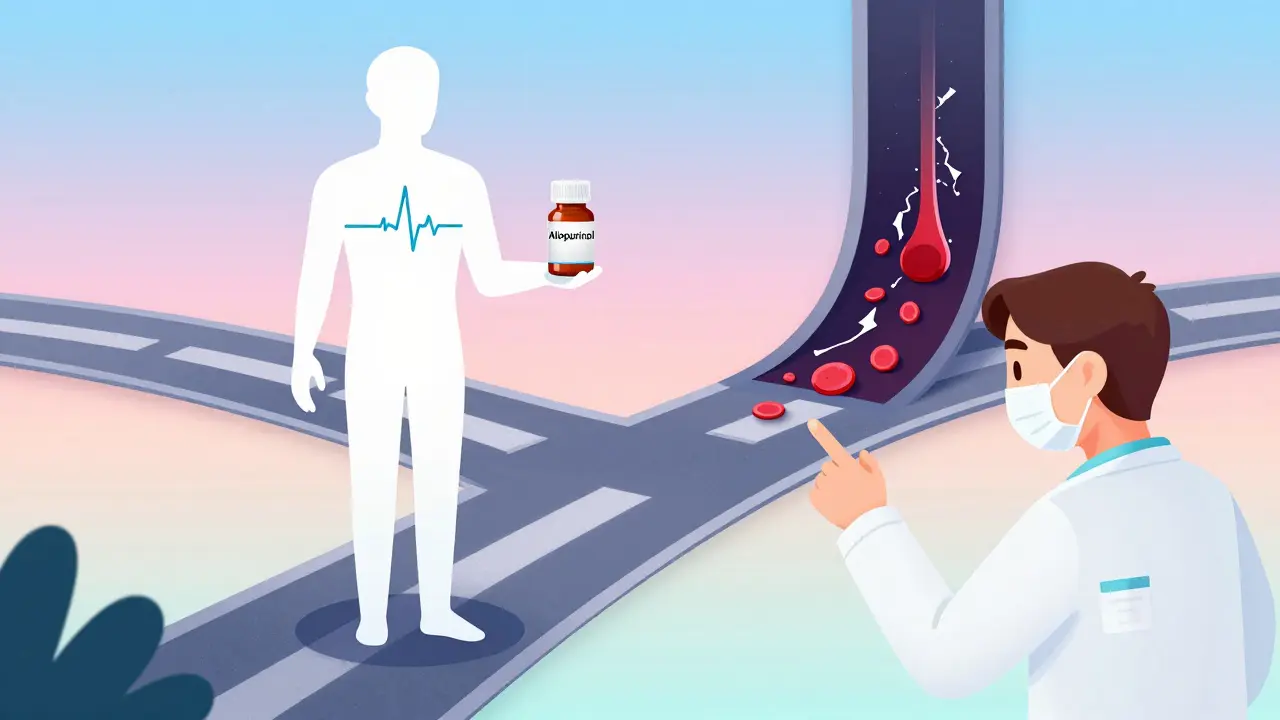
This tool checks if the combination of allopurinol and azathioprine could be dangerous for you. This interaction can cause severe bone marrow suppression and is potentially fatal.
Important Information
This tool provides educational information only. It does not replace professional medical advice. Always consult your healthcare provider before making any changes to your medication regimen.
What You Need to Know
When allopurinol is combined with azathioprine, the body cannot properly metabolize azathioprine. This causes levels of 6-mercaptopurine (6-MP) to increase by up to 4 times the normal amount, leading to severe bone marrow suppression.
Severe bone marrow suppression can cause:
- White blood cell counts below 1,100/mm³ (normal: 4,000-11,000)
- Neutrophil counts below 500/mm³
- Platelet counts below 20,000/mm³
Critical Warning
Combining these drugs can be fatal. It can cause severe bone marrow failure, leading to life-threatening infections, bleeding, and death.
What to do if you're on both medications:
- Stop taking both medications immediately and contact your doctor
- Seek emergency medical care if you experience fever, fatigue, bleeding, or easy bruising
- Get a complete blood count test immediately
- Do not restart either medication without specialist supervision
Combining allopurinol and azathioprine isn’t just risky-it can be deadly. This isn’t a hypothetical warning. It’s a well-documented, life-threatening interaction that has sent patients to the ICU, caused severe bone marrow failure, and led to hospital bills exceeding $50,000. And yet, it still happens-often because neither the patient nor the doctor realizes the danger.
Why This Interaction Is So Dangerous
Allopurinol is a common gout medication. It works by blocking xanthine oxidase, an enzyme that helps break down uric acid. Less uric acid means fewer painful gout flares. Azathioprine, on the other hand, is an immunosuppressant used for conditions like Crohn’s disease, ulcerative colitis, rheumatoid arthritis, and after organ transplants. It’s not a painkiller. It’s a powerful drug that shuts down parts of the immune system to stop inflammation. The problem starts when these two drugs meet. Allopurinol doesn’t just slow down uric acid production-it also blocks the body’s ability to break down azathioprine’s active form, 6-mercaptopurine (6-MP). When this happens, 6-MP builds up in the bloodstream. Levels can spike by up to four times what’s safe. That excess 6-MP gets turned into toxic compounds that attack the bone marrow. The result? Bone marrow suppression. White blood cells, red blood cells, and platelets crash. A patient might go from normal counts to a white blood cell count of 1,100/mm³ (normal is 4,000-11,000). Neutrophils-the body’s first line of defense against infection-can drop below 500/mm³. Platelets can fall below 20,000/mm³. That’s not just low. That’s dangerous. At these levels, even a minor cut can lead to uncontrolled bleeding. A cold can turn into pneumonia. An infection can become septic shock. One case from 1996, published in the New England Journal of Medicine, showed a 63-year-old heart transplant patient on azathioprine being prescribed allopurinol for wrist pain. Within weeks, he developed pancytopenia. His hemoglobin dropped to 3.7 g/dL (normal is 12-16). He needed four units of blood and a drug called GM-CSF just to restart his bone marrow. His hospital bill? $13,042 in 1996 dollars-over $25,000 today.How the Body Turns a Safe Drug Into a Poison
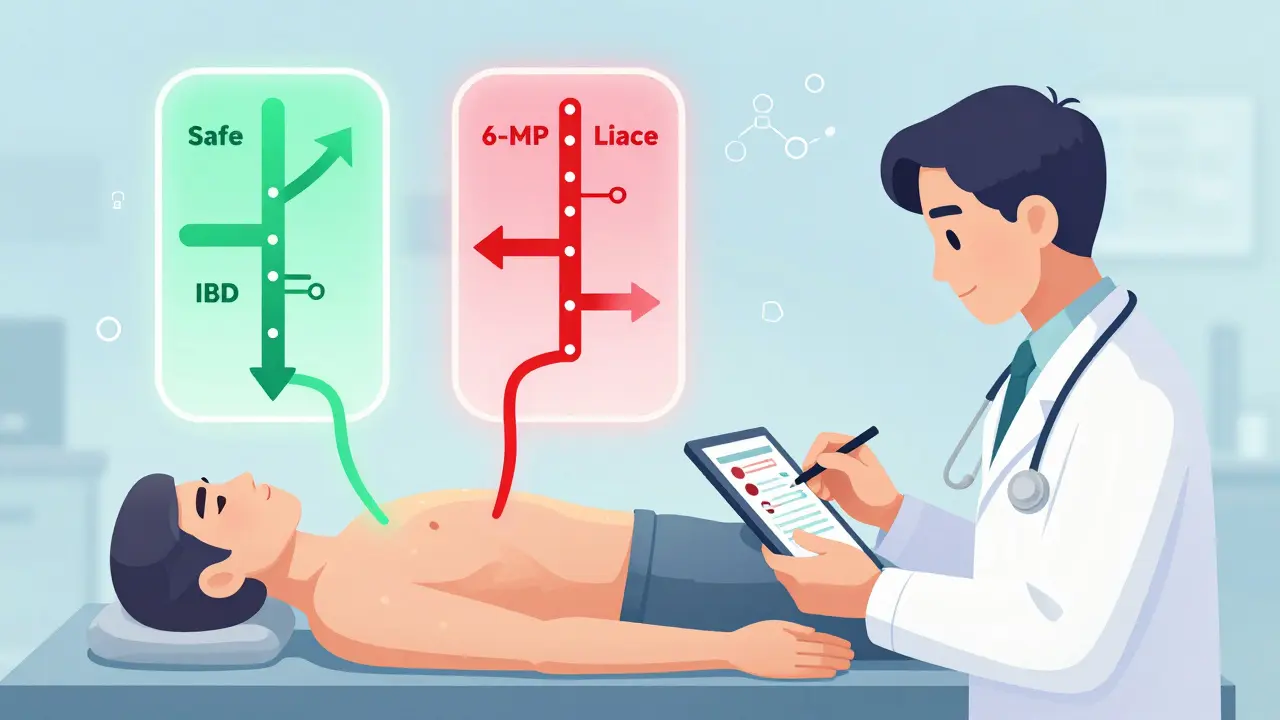
Azathioprine doesn’t work directly. It’s converted in the liver into 6-MP. From there, 6-MP has two main paths:- One path turns it into 6-thiouric acid, which is harmless and gets flushed out.
- The other turns it into thioguanine nucleotides (6-TGNs), which suppress the immune system-that’s the therapeutic effect.
When Doctors Might Still Prescribe Both (And How They Do It Safely)
Despite the risks, some specialists use this combination-on purpose. But only in very specific cases. About 25-30% of patients with inflammatory bowel disease (IBD) are “thiopurine shunters.” Their bodies convert too much azathioprine into 6-MMP, which causes liver damage instead of helping their gut. These patients don’t respond to standard doses. Their inflammation doesn’t improve. Their symptoms persist. And their livers get damaged. In these rare cases, doctors at specialized IBD centers may add low-dose allopurinol. But they don’t just slap it on. They follow a strict protocol:- Start azathioprine at 25-33% of the normal dose (usually 0.5-0.7 mg/kg/day instead of 2-2.5 mg/kg/day).
- Add allopurinol at 100 mg daily.
- Test blood levels of 6-TGN and 6-MMP before starting and every 4-8 weeks after.
- Keep 6-TGN between 230-450 pmol/8×10⁸ RBCs (the therapeutic range).
- Keep 6-MMP below 5,700 pmol/8×10⁸ RBCs (to avoid liver damage).
- Check complete blood counts weekly for the first month, then every two weeks for two months, then monthly.
What Happens If You Ignore the Warning
The risks aren’t theoretical. They’re real-and they’re happening right now. A 2021 survey of U.S. gastroenterologists found only 32% had ever used this combination. Why? Because the margin for error is razor-thin. One missed blood test. One delayed dose adjustment. One patient who didn’t understand the warning. And it’s over. Case reports keep coming. A 57-year-old man in 2022 developed severe myelosuppression after being prescribed allopurinol for gout while on azathioprine for autoimmune hepatitis. He spent three weeks in the hospital. His platelets were so low he needed transfusions. His white blood cells were nearly gone. He survived-but barely. And it’s not just about hospital stays. It’s about long-term damage. Bone marrow failure can lead to permanent blood disorders. Infections can cause organ damage. Some patients never fully recover their immune function. The FDA’s black box warning isn’t there for show. It’s the strongest warning they can give. It means: if you take azathioprine, never take allopurinol unless your doctor knows exactly what they’re doing.What You Should Do If You’re on Either Drug
If you’re taking azathioprine for Crohn’s, ulcerative colitis, rheumatoid arthritis, or after a transplant:- Do not take allopurinol without telling your specialist.
- Do not take over-the-counter gout remedies without checking with your doctor.
- Ask your pharmacist: “Is this safe with my current meds?”
- Get a blood test before starting any new drug-especially if you have joint pain.
- Ask your doctor: “Am I on any immunosuppressants?”
- If you’ve had a transplant, have IBD, or take meds for autoimmune disease, don’t assume allopurinol is safe.
- Report any signs of infection-fever, sore throat, fatigue-right away.
- Know your blood counts. Ask for your last CBC result.
Alternatives That Are Safer
You don’t have to choose between managing gout and staying alive. For gout:- Febuxostat works like allopurinol but doesn’t block xanthine oxidase the same way. It’s a safer option for people on azathioprine.
- Pegloticase is an IV infusion that breaks down uric acid directly. Used for severe, treatment-resistant gout.
- Colchicine prevents gout flares without affecting azathioprine metabolism.
- Methotrexate is often used instead of azathioprine.
- Biologics like adalimumab, infliximab, or vedolizumab don’t interact with allopurinol.
- Ustekinumab and risankizumab are newer options with no known interaction.
Final Warning
This interaction kills. It’s not rare. It’s preventable. But only if everyone involved-patient, pharmacist, doctor-knows the risk. If you’re on azathioprine, allopurinol is not a harmless add-on. It’s a red flag. A danger sign. A potential death sentence if ignored. And if you’re on allopurinol for gout, don’t assume your immune system is fine. Ask if you’re on any other meds that could turn this into a disaster. The science is clear. The guidelines are strict. The warnings are loud. Now it’s up to you to listen.Can I take allopurinol and azathioprine together if I lower the dose?
Only under strict specialist supervision. Even with dose reduction, the risk remains high. Azathioprine must be cut to 25-33% of the normal dose, and blood levels of 6-TGN and 6-MMP must be monitored weekly at first. This approach is only used in specialized IBD centers for patients who don’t respond to standard therapy. It is not safe for general use or primary care settings.
What are the signs of bone marrow suppression from this interaction?
Signs include unexplained fever, frequent infections, extreme fatigue, easy bruising or bleeding (like nosebleeds or gum bleeding), pale skin, and shortness of breath. These symptoms can develop quickly-sometimes within days. If you’re on either drug and notice any of these, get a blood test immediately.
Is febuxostat safer than allopurinol if I’m on azathioprine?
Yes. Febuxostat lowers uric acid but does not significantly inhibit xanthine oxidase in the same way allopurinol does. It does not cause the dangerous buildup of 6-MP. For patients on azathioprine, febuxostat is the preferred gout medication when uric acid-lowering is needed.
Why don’t more doctors know about this interaction?
Many doctors, especially general practitioners, aren’t trained in immunosuppressant metabolism. Allopurinol is seen as a simple gout drug. Azathioprine is often managed by specialists, but patients may see multiple providers. Without direct communication between specialists and GPs, the warning gets missed. That’s why patient awareness is critical.
Should I get genetic testing before taking azathioprine?
Yes. Testing for TPMT (thiopurine methyltransferase) enzyme activity can help predict how your body will process azathioprine. People with low or intermediate TPMT activity are at higher risk for bone marrow toxicity-even without allopurinol. While this test doesn’t eliminate the allopurinol risk, it helps identify who needs the closest monitoring.





Cassie Widders
January 12, 2026 AT 23:50Wow. I read this whole thing and just sat there stunned. This is the kind of stuff that should be on every med school syllabus.
People think gout is just a ‘rich man’s pain’ and azathioprine is just some ‘immune pill’ - but this? This is a silent killer hiding in plain sight.
I work in a pharmacy. I’ve seen this combo slip through. It’s terrifying.
Why isn’t there a mandatory alert in every EHR? This isn’t rare. It’s predictable. And we’re still letting it happen.
Faith Wright
January 13, 2026 AT 12:15So let me get this straight - we have a drug combo that can turn your bone marrow into a ghost town, and doctors still prescribe it like it’s a coffee refill?
Also, why are we even surprised? The system is designed to ignore chemistry and prioritize speed.
My aunt almost died from this. No one asked if she was on immunosuppressants. She just got a script for ‘gout pain’ and walked out.
Thanks for posting this. Someone needed to scream into the void.
Konika Choudhury
January 14, 2026 AT 10:00Why do Americans always make everything so complicated
in India we just take medicine and don’t overthink
if you get sick you go to doctor and take pill
why do you need 10 blood tests for one combo
you are too scared of your own bodies
Sona Chandra
January 15, 2026 AT 03:30THIS IS WHY AMERICA IS BROKEN
YOU TURN A SIMPLE MEDICATION INTO A SCIENCE FICTION MOVIE
ONE DRUG KILLS YOU IF YOU TAKE IT WITH ANOTHER
SO WHAT
DO YOU WANT A 50 PAGE PDF FOR EVERY PILL YOU SWALLOW
YOU PEOPLE ARE OUT OF YOUR MINDS
JUST DON’T MIX THEM IF YOU DON’T KNOW
IT’S NOT HARD
WHY IS EVERYTHING A CRISIS HERE
Amanda Eichstaedt
January 15, 2026 AT 20:24I’m a nurse who’s seen this play out twice.
First time: a 48-year-old woman with RA on azathioprine gets allopurinol for gout. Two weeks later, she’s in the ER with a fever of 104, no white cells, and a platelet count of 12,000.
Second time: a 61-year-old man with Crohn’s - same story.
Both survived. Both needed months of recovery.
And both were told by their PCPs: ‘It’s just a gout pill.’
It’s not. It’s a grenade with the pin pulled.
And no one’s training GPs on this. That’s the real tragedy.
Rinky Tandon
January 15, 2026 AT 22:21TPMT genotyping is mandatory in EU for thiopurine initiation and yet here in the US you’re still playing Russian roulette with bone marrow
the pharmacogenomic literacy gap is criminal
primary care providers are being asked to manage complex metabolic pathways without the tools or training
and we wonder why iatrogenic disasters are rising
it’s not negligence it’s systemic abandonment of clinical pharmacology
you can’t outsource pharmacokinetics to Google
Alex Fortwengler
January 17, 2026 AT 01:07They don’t want you to know this.
Big Pharma knows this interaction kills. But they don’t care. Why?
Because allopurinol is generic. Cheap. Easy to prescribe.
Azathioprine? Also generic. But febuxostat? Expensive. Patent protected.
They’d rather you die slowly than lose a billion in sales.
And the FDA? They’re just a rubber stamp.
This isn’t a medical error. It’s a profit-driven massacre.
Ask yourself - who profits when you need a transplant because your bone marrow got wiped out?
Darryl Perry
January 17, 2026 AT 13:41Stop dramatizing.
It’s a known interaction.
Pharmacists flag it.
Doctors check EHRs.
Patients read labels.
If you can’t handle that, don’t take meds.
Not every drug interaction needs a 2000-word essay.
Just don’t mix them.
Simple.
TiM Vince
January 17, 2026 AT 20:36My dad was on azathioprine for ulcerative colitis. He got gout. His doctor prescribed allopurinol. He didn’t know the risk. Neither did the pharmacist.
He didn’t die - but he spent three weeks in the hospital. Lost 30 pounds. Couldn’t work for six months.
Now he won’t take anything without asking me to check it.
I’m 29. I shouldn’t have to be my dad’s drug safety officer.
But here we are.
Katherine Carlock
January 19, 2026 AT 18:05Okay but can we just pause for a second and appreciate how wild it is that we’ve known about this since the 90s and yet it still happens?
Like - we have the science. We have the data. We have the guidelines.
But we still don’t have a system that works.
It’s not about the drugs. It’s about the people.
Doctors are overworked.
Pharmacists are understaffed.
Patients are overwhelmed.
We’re all just trying to survive the system.
And this interaction? It’s the canary in the coal mine.
Someone’s gotta speak up.
Thanks for speaking.
jordan shiyangeni
January 20, 2026 AT 09:47It is not merely a matter of pharmacokinetic interference; it is a systemic failure of medical education, clinical decision support infrastructure, and patient-centered communication.
The xanthine oxidase enzyme is not merely an incidental metabolic pathway - it is a critical regulatory node in thiopurine homeostasis.
When allopurinol inhibits this enzyme, the metabolic shunt toward 6-TGN accumulation is not a ‘side effect’ - it is a biochemical inevitability.
And yet, in the majority of primary care settings, this interaction remains unflagged, unmonitored, and unacknowledged.
Until we institutionalize pharmacogenomic screening and mandate interdisciplinary review for all thiopurine prescriptions - this will continue to happen.
And when it does, it will not be an accident.
It will be negligence.
And negligence, in medicine, is murder by omission.
Abner San Diego
January 20, 2026 AT 11:16Let’s be real - this is why I don’t trust doctors.
They treat gout like it’s a minor annoyance and don’t even ask what else you’re on.
My cousin’s husband got this combo. He was fine one day. Three weeks later, he was in ICU with no blood cells.
They gave him a transfusion. Then another. Then a shot to wake up his marrow.
He’s alive. But he’s never the same.
And the doctor? He just shrugged and said, ‘I didn’t know he was on that.’
Well now you know.
So do your job.
Lelia Battle
January 20, 2026 AT 13:30There is a quiet tragedy in modern medicine: we treat drugs as discrete entities, forgetting they exist within a living, dynamic system.
Allopurinol and azathioprine are not just molecules - they are actors in a biochemical drama, each with roles, pathways, and consequences.
When we reduce pharmacology to ‘don’t mix these,’ we ignore the deeper truth: the body is not a machine with interchangeable parts.
It is a conversation - and some conversations, once interrupted, never recover.
This is why humility must precede prescription.
Not certainty.
Not speed.
But humility.
Daniel Pate
January 22, 2026 AT 09:32If febuxostat is safer, why isn’t it the first-line treatment for gout in patients on azathioprine? Is it cost? Lack of awareness? Or just inertia?
And why is this interaction still not a mandatory alert in every EHR? We have AI that can recommend cat breeds based on photos - but we can’t flag a lethal drug combo?
What does that say about our priorities?
And more importantly - who’s responsible for fixing it?
Not the patient.
Not the pharmacist.
It’s the system.