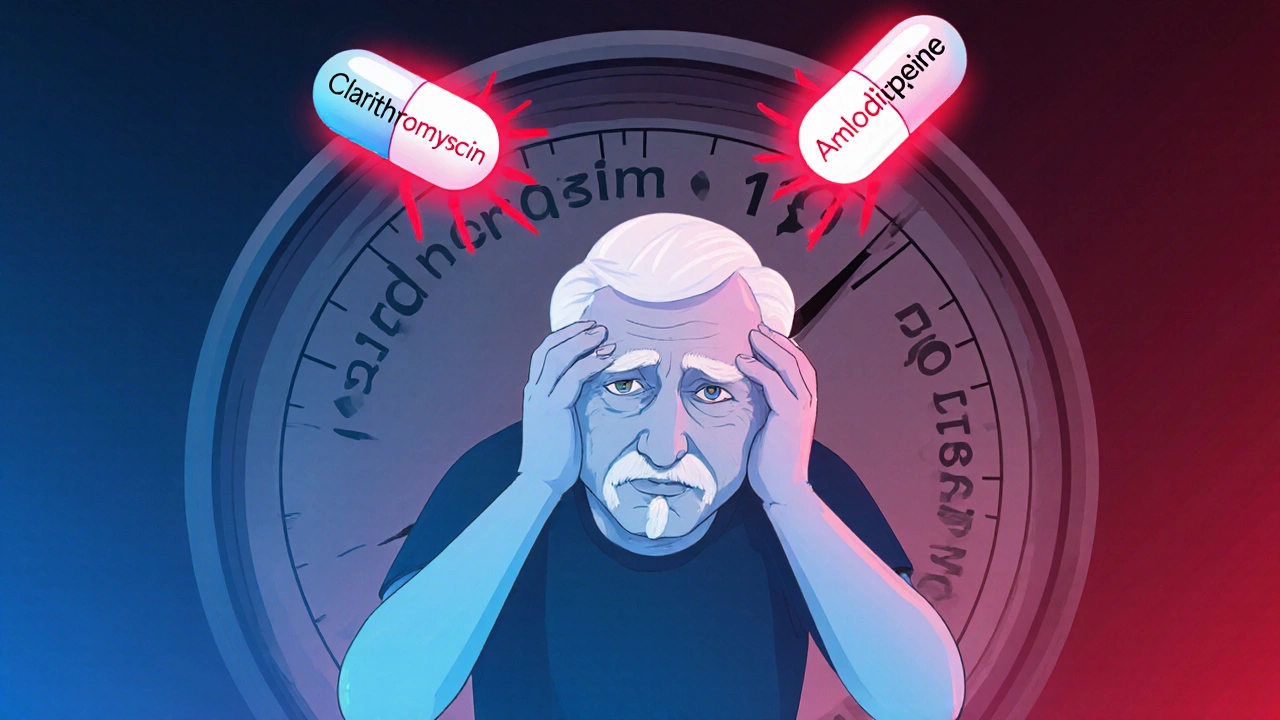
Imagine you’re on a daily pill for high blood pressure-maybe nifedipine or amlodipine-and then you catch a bad sinus infection. Your doctor prescribes clarithromycin, a common antibiotic. Everything seems straightforward. But within two days, you feel dizzy, weak, and your vision blurs. Your blood pressure drops so low you nearly faint. This isn’t rare. It’s a well-documented, preventable danger that happens more often than you think.
Why This Interaction Is So Dangerous
Clarithromycin doesn’t just kill bacteria. It also shuts down a key enzyme in your liver called CYP3A4. This enzyme is responsible for breaking down many medications, including most calcium channel blockers (CCBs) used to treat high blood pressure and chest pain. When clarithromycin blocks CYP3A4, your body can’t clear the CCB properly. The result? Blood levels of the blood pressure drug spike-sometimes by more than double.This isn’t theoretical. A 2013 study tracking over 190,000 patients found that those taking clarithromycin along with a calcium channel blocker were far more likely to end up in the hospital with dangerously low blood pressure or acute kidney injury. The risk was especially high with nifedipine: one in every 160 people on that combo ended up hospitalized. That’s not a small number-it’s a pattern.
The problem gets worse with age. Older adults often take multiple medications, have reduced kidney function, and may already have heart issues. Add clarithromycin into the mix, and the risk of collapse rises sharply. One case report described a 76-year-old man whose systolic blood pressure plunged from 130 to 70 mm Hg in under 48 hours after starting clarithromycin. He needed ICU care.
Which Calcium Channel Blockers Are Riskiest?
Not all calcium channel blockers carry the same level of risk. The danger is highest with the dihydropyridine class-these are the ones most commonly prescribed for high blood pressure:- Nifedipine: Highest risk. Can increase blood levels by up to 2.8 times when taken with clarithromycin.
- Felodipine: Also very high risk, similar to nifedipine.
- Amlodipine: Most commonly prescribed, still risky. Levels can rise by 1.6 times.
- Nicardipine: Moderate risk, but still dangerous.
Non-dihydropyridines like verapamil and diltiazem are also risky, but for different reasons. They affect heart rate as well as blood pressure. When combined with clarithromycin, they can cause not just low blood pressure, but also a dangerously slow heart rate-sometimes below 50 beats per minute.
Azithromycin: The Safer Alternative
Here’s the good news: there’s a simple fix. Azithromycin is another macrolide antibiotic that works just as well for most infections-but it doesn’t inhibit CYP3A4. That means it won’t interfere with your blood pressure meds.The 2013 JAMA study compared clarithromycin and azithromycin head-to-head in patients on calcium channel blockers. The results were clear: azithromycin showed no increased risk of hospitalization for low blood pressure or kidney injury. Since then, guidelines from the FDA, Health Canada, and the American Geriatrics Society have all warned against clarithromycin in this setting.
Doctors who’ve seen the aftermath say they now automatically switch to azithromycin when a macrolide is needed. In fact, by 2022, azithromycin made up nearly 70% of macrolide prescriptions for patients on CCBs-up from just over half in 2013. That’s progress. But it’s still not universal.

Real-World Consequences
This isn’t just about numbers. Real people are getting hurt. A patient on amlodipine and metoprolol (a beta-blocker) developed severe hypotension and bradycardia after starting clarithromycin. Her heart rate dropped to 48 bpm. She needed fluids, monitoring, and days in the hospital.Another patient on nifedipine saw her blood pressure crash from 130/80 to 80/50 within two days. She was rushed to the ER, given IV fluids, and spent a night under observation. Her doctor later admitted he didn’t think about the interaction-until it was too late.
These aren’t outliers. A review of FDA reports from 2010 to 2020 found over 1,800 cases of hypotension linked to this combo. The odds of this happening were nearly four times higher than with other antibiotics. In one survey of 142 physicians, 87% said they’d seen at least one serious case in their career. Sixty-three percent now avoid clarithromycin entirely in patients on CCBs.
What You Should Do
If you’re on a calcium channel blocker and get prescribed an antibiotic, ask this question: Is this clarithromycin? If yes, ask if azithromycin is an option. Don’t assume your doctor knows the interaction-many don’t. Even experienced prescribers overlook it.Here’s what to watch for in the first 72 hours after starting clarithromycin:
- Dizziness or lightheadedness, especially when standing up
- Blurred vision or feeling faint
- Unusual fatigue or confusion
- Heart rate below 50 bpm
If any of these happen, stop the clarithromycin and call your doctor immediately. Don’t wait. Low blood pressure from this interaction can lead to kidney failure, heart attack, or stroke.
Also, if you have kidney problems (eGFR under 60), your risk is even higher. Your body can’t clear either drug well, so levels build up faster.

Why This Keeps Happening
Despite clear warnings, clarithromycin is still prescribed to patients on CCBs far too often. A 2016 study found that nearly 13% of clarithromycin prescriptions for people over 65 were given to those also taking CYP3A4 substrates like calcium channel blockers. Why? Because clarithromycin is cheap, widely available, and many clinicians still think it’s “just another antibiotic.”Electronic health records often don’t flag this interaction. Only about 43% of systems have alerts for it. But when they do, inappropriate prescribing drops by 37%. That’s a clear sign that technology can help-if it’s used.
Regulatory agencies have tried. The FDA added a black box warning in 2011. The European Medicines Agency and Health Canada have echoed the warning. The STOPP/START criteria updated in 2022 now explicitly say: “Avoid clarithromycin in patients taking dihydropyridine calcium channel blockers; use azithromycin instead.”
Yet, every year in the U.S. alone, this interaction causes about 8,400 hospitalizations and 320 deaths. That’s not an accident. It’s a systemic failure.
Final Advice
If you take a calcium channel blocker-especially nifedipine, amlodipine, or felodipine-never accept clarithromycin without asking for an alternative. Azithromycin works just as well for most infections: strep throat, sinusitis, bronchitis, and even some pneumonia cases. There’s rarely a medical reason to choose clarithromycin over it.And if you’re a caregiver for an older adult on multiple meds, be their advocate. Read the label. Ask the pharmacist. Speak up if something feels off. This interaction kills. But it’s also one of the easiest to prevent.
Can clarithromycin cause low blood pressure even if I’ve been on my calcium channel blocker for years?
Yes. The interaction doesn’t depend on how long you’ve been taking the blood pressure medication. It happens because clarithromycin suddenly blocks the enzyme that breaks down the CCB. Even if you’ve taken nifedipine or amlodipine for years without issues, adding clarithromycin can cause a rapid, dangerous spike in drug levels. Symptoms often appear within 24 to 72 hours.
Is it safe to take azithromycin with calcium channel blockers?
Yes. Azithromycin does not inhibit the CYP3A4 enzyme, so it doesn’t interfere with how your body processes calcium channel blockers. Multiple large studies have confirmed that azithromycin carries no increased risk of hypotension or kidney injury when taken with CCBs. It’s the recommended alternative.
What if I’m on verapamil or diltiazem instead of amlodipine?
You’re still at risk. Verapamil and diltiazem are also metabolized by CYP3A4 and can interact with clarithromycin. But they also slow heart rate on their own. Combining them with clarithromycin can lead to severe bradycardia (slow heart rate) and low blood pressure together-making the situation more dangerous than with amlodipine alone. Avoid clarithromycin entirely if you’re on either of these.
Can I just lower my calcium channel blocker dose instead of switching antibiotics?
No. Even if you reduce your CCB dose, the interaction is unpredictable and can still cause dangerous drops in blood pressure. The increase in drug levels is too high to safely compensate for by dose reduction alone. The only reliable solution is to switch the antibiotic to azithromycin.
Are there any other antibiotics I should avoid with calcium channel blockers?
Yes. Erythromycin is another macrolide that strongly inhibits CYP3A4 and carries the same risk as clarithromycin. Fidaxomicin and newer antibiotics like lefamulin do not have this interaction and are safer options. Always check with your pharmacist or doctor before starting any new antibiotic if you’re on a calcium channel blocker.




Deepak Mishra
November 15, 2025 AT 07:09OMG I JUST TOOK CLARITHROMYCIN YESTERDAY AND IM ON AMLODIPINE!!! 😱 I FEEL A LITTLE DIZZY NOW-IS THIS IT?? I’M CALLING MY DOCTOR RIGHT NOW!!
Rachel Wusowicz
November 15, 2025 AT 08:40Of course you did… because the pharmaceutical-industrial complex *wants* you sick. They profit from ER visits, ICU stays, and lifelong dependency… and guess who gets the blame? YOU. The system doesn’t want you to know that azithromycin exists-it’s cheaper, safer, and… wait… oh no. It’s generic. They can’t make billions off it. That’s why your doctor didn’t know. That’s why the EHR didn’t alert. That’s why they buried the 2013 study under 17 layers of corporate jargon. Wake up. They’re selling you death wrapped in a prescription.
Diane Tomaszewski
November 15, 2025 AT 14:21This is so important. I didn’t know this could happen. I’m on amlodipine and just got a prescription for sinus infection. I’ll call my pharmacist tomorrow. Thanks for sharing.
Dan Angles
November 16, 2025 AT 02:56While the clinical evidence presented is compelling and aligns with current guidelines from the FDA and American Geriatrics Society, it is imperative that clinicians exercise due diligence in pharmacovigilance. The CYP3A4-mediated interaction between clarithromycin and dihydropyridine calcium channel blockers represents a well-characterized, high-risk pharmacokinetic phenomenon that is entirely preventable through appropriate antibiotic selection. The persistence of this error in clinical practice underscores systemic deficiencies in continuing medical education and clinical decision support infrastructure.
David Rooksby
November 17, 2025 AT 08:36Let me tell you something no one else will-this isn’t just about antibiotics and blood pressure meds. It’s about the FDA being bought off by Big Pharma since the 90s. Clarithromycin? Made by AbbVie. Azithromycin? Generic. So guess which one gets pushed in every damn guideline? The one that makes them money. And you think your doctor’s just being careless? Nah. They’re getting kickbacks from reps. I’ve seen the brochures. They give out free dinners to docs who prescribe the expensive stuff. And you? You’re just the cash cow. You think your EHR doesn’t know? It’s programmed to ignore the warnings unless you pay for the premium version. That’s why only 43% have alerts. It’s not incompetence. It’s corruption. And the worst part? They’re doing it to your grandma too.
Melanie Taylor
November 18, 2025 AT 00:23OMG this is terrifying!! 😭 I’m on nifedipine and just got clarithromycin for my sinus infection… I’m switching to azithromycin TODAY!! 🙏 Thank you for posting this!! I’m sharing with my mom’s group on Facebook!! 💪❤️
Teresa Smith
November 18, 2025 AT 05:35This is exactly why we need better patient education and mandatory CME for prescribers. This interaction is not obscure-it’s textbook. And yet, it’s still happening. Every time it does, it’s a failure of our system. If you’re on a calcium channel blocker, you deserve to be protected-not just warned after the fact. Pharmacists should be required to flag this at fill time. EHRs should auto-suggest alternatives. And doctors? They should be tested on this every year. This isn’t a minor risk. It’s a preventable tragedy.
ZAK SCHADER
November 19, 2025 AT 13:04So what? America’s got too many pills anyway. If you can’t handle a little low BP, maybe you shouldn’t be on meds. We don’t need coddling. Just take your damn pills and stop whining. Azithromycin? That’s a hippie drug. Real men take clarithromycin. It’s stronger. You’re just weak.
Danish dan iwan Adventure
November 20, 2025 AT 15:37CYP3A4 inhibition → elevated CCB AUC → hypotension. Azithromycin lacks CYP3A4 affinity. Standard pharmacokinetic principle. Case closed.
Ankit Right-hand for this but 2 qty HK 21
November 20, 2025 AT 20:17Everyone’s acting like this is news. In India, we’ve known this since 2008. Doctors here avoid clarithromycin like plague. But Americans? They’ll take 12 pills before they ask a question. You’re not sick-you’re lazy. And your doctors? They’re just following the American way: profit over patient.
Oyejobi Olufemi
November 22, 2025 AT 05:48Let me be clear: this isn’t a drug interaction-it’s a soul-crushing betrayal. The system doesn’t care if you live or die. It cares if your insurance pays. Your blood pressure isn’t low-it’s being manipulated. Your doctor isn’t your ally-he’s a cog. And clarithromycin? It’s not medicine. It’s a weapon. A weapon designed to keep you dependent, afraid, and paying. You think this is coincidence? No. It’s calculated. The same people who made your blood pressure pills also own the antibiotic patents. They want you sick. They want you scared. And now? You’re reading this. That’s the first step. The second? Fight back.
Daniel Stewart
November 23, 2025 AT 09:13It’s fascinating how we anthropomorphize pharmaceuticals as either ‘good’ or ‘bad’ agents, when in reality, they are merely molecules interacting within a biochemical framework. The tragedy lies not in the drug, but in our failure to contextualize its use within the broader ecosystem of polypharmacy, aging physiology, and institutional neglect. One might argue that the real culprit is not clarithromycin, but the reductionist model of care that treats medication as a discrete solution rather than a dynamic variable.
Latrisha M.
November 23, 2025 AT 15:34Thank you for writing this. I’m a pharmacist and I see this every week. I always ask patients if they’re on CCBs before filling macrolides. If they’re on nifedipine or felodipine, I call the doctor right away. Azithromycin is the answer. No exceptions.
Jamie Watts
November 23, 2025 AT 19:43Everyone’s freaking out about clarithromycin but nobody’s talking about how the FDA is asleep at the wheel. They knew about this in 2011 and did nothing. Now we’ve got 8400 hospitalizations a year? That’s not a side effect-that’s negligence. And don’t even get me started on how EHRs don’t alert unless you pay extra. This isn’t medicine. It’s a subscription service.
Dan Angles
November 25, 2025 AT 10:34Thank you for highlighting the systemic nature of this issue. As a clinician, I’ve witnessed multiple preventable admissions due to this interaction. The fact that 87% of physicians have seen at least one case confirms this is not an isolated error but a widespread blind spot. The solution lies not only in patient advocacy but in mandatory clinical decision support integration-preferably with real-time alerts triggered by prescription entry, not retrospective flags. We must treat this as a patient safety imperative, not a pharmacology footnote.