How much does a 30-day supply of metformin cost? What about lisinopril? If you’re a doctor, chances are you don’t know the exact price - and you’re not alone. Despite prescribing these drugs every day, most clinicians grossly misestimate what patients actually pay out of pocket. A 2016 study of 254 doctors and medical students found that only 5.4% of generic drug costs were estimated within 25% of the actual price. For brand-name drugs, it was slightly better - but still shockingly low at 13.7%. And here’s the kicker: doctors consistently overestimated cheap drugs by nearly 80% and underestimated expensive ones by more than half.
Why This Gap Matters More Than You Think
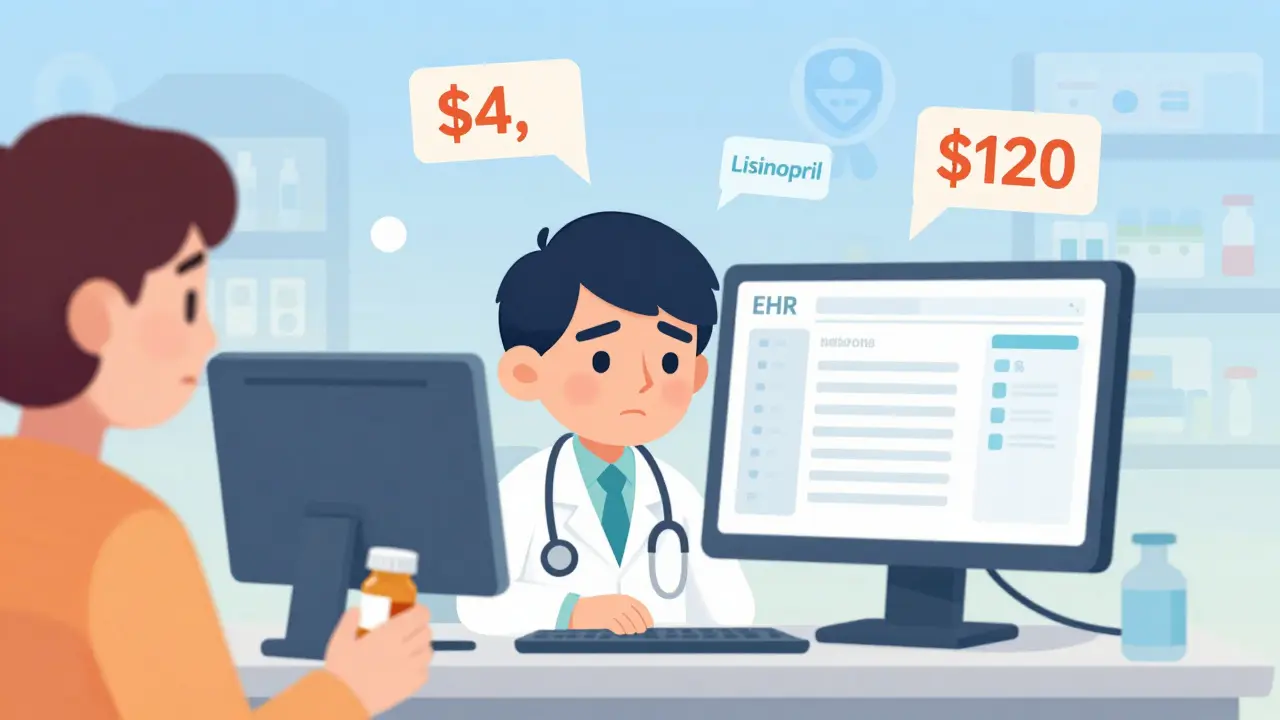
It’s not just about being wrong on a quiz. When a clinician doesn’t know the price of a medication, they’re making decisions in the dark. A patient walks in with high blood pressure. The doctor prescribes a brand-name ACE inhibitor because it’s what they learned in med school. The patient fills the script - and then skips doses because the copay is $120 a month. Three months later, they’re back in the ER with a stroke. That’s not hypothetical. It happens every day. The American Medical Association calls cost-conscious prescribing a professional responsibility. But how can you be cost-conscious if you don’t know the cost?
The U.S. spends $621 billion a year on prescription drugs. That’s nearly 10% of all healthcare spending. And 28% of adults say they’ve skipped or cut pills because they couldn’t afford them. The disconnect isn’t just between patient and pharmacy - it’s between the prescriber and the real world. Clinicians are trained to think about efficacy, side effects, and drug interactions. Price? That’s treated like a billing department problem. But when patients can’t afford the medicine, efficacy doesn’t matter.
What Clinicians Get Wrong - And Why
Research shows a pattern: inexpensive generics are seen as expensive. Expensive brand-name drugs are seen as cheaper than they are. Why? Because most doctors never see the actual price. They see the wholesale acquisition cost (WAC) listed in a textbook - which has nothing to do with what a patient pays. A generic version of glipizide might cost $4 at Walmart, but if your training only showed you the $40 WAC from 10 years ago, you’ll assume it’s still $30-$40. Meanwhile, a new diabetes drug like semaglutide might cost $1,000 a month, but if you only hear about it in a drug rep’s pitch, you might think it’s “only” $300.
Another problem? Doctors think drug prices reflect R&D costs. They’re wrong. A 2023 KFF survey found that 50% of the public believes high prices are due to research and development. But among medical students? Only 44% knew that’s not true. In reality, most price hikes happen after patents expire, with manufacturers raising prices on older drugs with no clinical improvement. Humira’s price jumped 4.7% in 2023 - even though it had no new indications. That’s not innovation. That’s profit.
The EHR Fix - And Why It’s Not Working Yet
Enter electronic health records. In 2021, a JAMA Network Open study showed that when clinicians had real-time out-of-pocket cost data pop up in their EHR during prescribing, they got better at estimating prices. Even better - one in eight changed their prescription because of it. If the potential savings were over $20, that number jumped to one in six.
So why aren’t all clinics using this? Because it’s messy. UCHealth spent 18 months and $2.3 million building a system that pulls in real-time pricing from pharmacies and insurance plans. But even then, it’s not perfect. One internal medicine resident on Reddit said: “The cost alerts show insurer pricing, but not my patient’s actual copay. So I pick a cheaper drug - and the patient still pays $90 because their plan has a weird deductible.”
There are also technical barriers. The same drug can cost $15 at one pharmacy and $320 at another. EHRs often pull from a single source, so the number you see might be useless for the patient sitting in front of you. And if the alert pops up after you’ve already typed the prescription? Most doctors just click through. They’re already running 20 minutes behind.

Who’s Getting It Right - And Who’s Falling Behind
Age matters. Doctors under 40 are 50% more likely to use cost tools than those over 55. Why? They grew up with tech. They’re used to checking prices before buying anything. Older clinicians? They remember when drugs were $5. They don’t expect to need a calculator to prescribe.
Training matters too. Only 44% of U.S. medical schools have formal drug pricing curriculum. That means most doctors graduate without ever learning how to find or interpret drug costs. Meanwhile, institutions like Mayo Clinic have built internal Drug Cost Resource Guides - updated quarterly - that clinicians rate 4.7 out of 5. Compare that to the generic Medicare Part D formulary, rated 2.8. One is a living tool. The other is a PDF nobody reads.
And then there’s the safety-net clinics. Early data from Harvard and UCHealth’s joint study shows that in clinics serving low-income patients, cost alerts led to 22% more prescription changes than in private practices. Why? Because those doctors already know their patients are skipping doses. They’re not just prescribing - they’re problem-solving. And when cost data is right there, they act.
The Bigger Picture: Policy Is Catching Up
Change isn’t just coming from the clinic. It’s coming from Washington. The 2022 Inflation Reduction Act let Medicare negotiate prices on 10 high-cost drugs. That number will rise to 15 in 2025. Eighty percent of Americans - across party lines - support this. And now, CMS requires drugmakers to report out-of-pocket cost estimates. That’s new. That’s meaningful.
But here’s the truth: policy won’t fix this alone. Even if Medicare negotiates a drug down to $50, if the doctor doesn’t know that’s the new price, they’ll still write the $300 brand-name version. The system needs both policy and point-of-care tools. And education. Real education.

What Needs to Change - Right Now
Here’s what works:
- Cost alerts in EHRs - but only if they show patient-specific copays, not just list prices.
- Integration with pharmacy networks - so the system knows what the local CVS, Walgreens, or community pharmacy charges.
- Training in med school and residency - not as an elective, but as core curriculum. Teach students how to use GoodRx, NeedyMeds, and their own EHR’s pricing tool.
- Feedback loops - if a doctor prescribes a drug and the patient can’t afford it, the system should notify them. Not as punishment - as learning.
It’s not about making doctors cost-cutters. It’s about making them informed decision-makers. A good doctor doesn’t pick the cheapest drug. They pick the right drug - at a price the patient can afford. That’s value-based care. And it starts with knowing the price.
What’s Next?
By 2027, 75% of U.S. health systems are projected to have advanced real-time benefit tools. That’s progress. But progress won’t help if the tools are inaccurate, slow, or ignored. The next step isn’t just better tech - it’s better culture. Clinicians need to feel empowered, not burdened. Patients need to know their doctors are fighting for them - not just writing scripts.
The data is clear: clinicians don’t know drug prices. And that’s costing lives. Fixing it won’t be easy. But it’s necessary. Because if you don’t know how much something costs, you can’t truly care about whether someone can get it.
Do most doctors know how much their prescriptions cost?
No. Studies show most clinicians misestimate drug prices - often by a large margin. Generic drugs are typically overestimated, while expensive brand-name drugs are underestimated. Only about 5% of generic drug costs and 14% of brand-name drug costs are estimated within 25% of the actual price.
Why don’t clinicians know drug prices?
Most medical schools don’t teach drug pricing. Clinicians rarely see actual patient out-of-pocket costs during training. They rely on outdated textbook prices or wholesale costs, which don’t reflect what patients pay. Plus, pricing varies wildly by pharmacy, insurance, and location - making it nearly impossible to memorize.
Can EHR cost alerts help doctors prescribe more affordably?
Yes - but only if they’re accurate and easy to use. Studies show that when EHRs show real-time, patient-specific copay estimates, one in eight doctors change their prescription. That number rises to one in six when potential savings exceed $20. But many systems show insurer pricing, not actual patient costs, leading to confusion and distrust.
Is drug pricing taught in medical school?
Only in about 44% of U.S. medical schools. Most students graduate without formal training on how to find, interpret, or use drug pricing information. This gap contributes to persistent misestimation and poor cost-conscious prescribing habits.
Do drug prices reflect research and development costs?
No - and most people, including doctors, think they do. In reality, price increases often happen after patents expire, with no clinical improvement. For example, Humira’s price rose 4.7% in 2023 despite no new indications. Research and development costs are only one small part of the final price.
What’s being done to fix this problem?
The Inflation Reduction Act lets Medicare negotiate prices on high-cost drugs. CMS now requires manufacturers to report out-of-pocket costs. Some hospitals, like Mayo Clinic and UCHealth, have built internal cost tools with high user satisfaction. But adoption is still low - only 37% of U.S. health systems use real-time benefit tools as of late 2024.





RAJAT KD
January 8, 2026 AT 14:56Doctors prescribing drugs they don't understand the cost of is like a chef cooking without tasting. It's not negligence-it's systemic failure.
Jeffrey Hu
January 9, 2026 AT 11:09Let’s be real-this isn’t about education. It’s about laziness. If you’re too busy to check GoodRx before hitting ‘prescribe,’ you shouldn’t be writing scripts. I’ve seen residents spend 20 minutes debating side effect profiles but 10 seconds on cost. Pathetic.
Drew Pearlman
January 10, 2026 AT 00:30I get it. We’re all drowning in EHR pop-ups, alerts, and checkboxes. But here’s the thing-when you see a patient’s face drop because they can’t afford their insulin, it sticks with you. I used to think pricing was a pharmacy problem. Then I had a 72-year-old widow cry because she was splitting her metformin pills. Now? I check NeedyMeds before I even open the chart. It’s not just better medicine-it’s human medicine.
And yeah, the EHR tools are clunky. But they’re getting better. My clinic just integrated real-time copay data from our local pharmacy chain, and guess what? We’ve cut high-cost prescriptions by 31% in six months. No magic. Just data. And care.
It’s not about being a cost-cutter. It’s about being a problem-solver. If your patient can’t afford the script, it’s not a prescription-it’s a suggestion. And suggestions don’t save lives.
Micheal Murdoch
January 11, 2026 AT 05:39What’s wild is how many of us still think drug pricing is about innovation. I used to believe that too-until I saw the patent cliff charts. Humira’s price went up 4.7% last year? No new indications. No new science. Just a corporation deciding they could. And we’re the ones who pay for it-with our health, our time, our dignity.
Med school didn’t teach me this. Pharma reps didn’t tell me this. But patients did. Every time they said, ‘I’ll just wait till payday.’ Every time they skipped doses because the copay was more than their grocery budget.
Real cost-conscious care isn’t about picking the cheapest drug. It’s about asking, ‘What can this person actually take?’ And then having the tools to make that happen. We’re not just doctors. We’re gatekeepers. And right now, our gate is broken.
Fixing this isn’t political. It’s ethical. And it starts with a single question: ‘How much will this cost you?’
Jacob Paterson
January 12, 2026 AT 03:06Oh please. So now doctors are victims of bad tech? Let me guess-you also blame the EHR when your patient has a heart attack because you forgot to check their meds. Wake up. If you can’t remember that lisinopril is $4, you’re not a doctor-you’re a glorified order-taker. And your patients are paying the price.
GoodRx exists. NeedyMeds exists. Your hospital has a cost tool. But you’d rather click ‘next’ than think. That’s not a system failure. That’s moral failure.
tali murah
January 14, 2026 AT 01:22Let’s be brutally honest: this isn’t about patients. It’s about profit. The system is designed to keep you blind. Why? Because if doctors knew how much drugs *actually* cost, they’d stop prescribing them. And that would cut into margins. So they train you on mechanisms, not money. They give you flashy slides on pharmacokinetics but zero data on copays. It’s not incompetence-it’s indoctrination.
And don’t get me started on ‘EHR alerts.’ They’re theater. A pop-up that says ‘$120’ when the patient’s deductible is $5,000? That’s not helpful. That’s cruel. It’s like giving a starving person a menu with no prices.
The real solution? Ban brand-name prescribing unless the patient has a documented reason. Let generics be the default. Make cost education mandatory. And fire every doctor who still thinks ‘it’s just a copay.’
Lindsey Wellmann
January 15, 2026 AT 15:16OMG I CRIED reading this. 😭 Like… I’m a nurse and my best friend’s mom skipped her blood pressure med for 3 months because she thought it was $150 a month… and it was $8 at Walmart. She almost had a stroke. 😭 This is NOT okay. We need to fix this. Like, NOW. 🙏 #HealthcareIsAHumanRight
Matthew Maxwell
January 17, 2026 AT 09:29There is no excuse for this level of professional negligence. Medical education has been watered down to the point where clinicians are functionally illiterate in basic economic realities. If you cannot accurately estimate the cost of a $4 generic, you are unfit to practice. This is not a systemic issue-it is a failure of character. The AMA should revoke licenses for such incompetence.
Chris Kauwe
January 18, 2026 AT 18:35Let’s cut through the woke noise. The real problem isn’t that doctors don’t know prices-it’s that we’ve allowed a broken, corporatized healthcare system to replace clinical judgment with bureaucratic noise. EHR alerts? GoodRx? These are Band-Aids on a hemorrhage. The root issue is the destruction of the doctor-patient relationship by insurance middlemen, patent monopolies, and regulatory capture. We need to dismantle the pharmaceutical-industrial complex, not slap a price widget on our EMR.
And yes-some of us older docs remember when a prescription cost $5. We didn’t need an app. We had trust. And we knew our patients. That’s what’s missing. Not data. Humanity.
Pooja Kumari
January 19, 2026 AT 05:36I’m from India, and I’ve seen this in both countries. In the U.S., it’s the silence. No one talks about cost because it’s too painful. In India, it’s the screaming-patients begging for cheaper options, doctors scrambling to find generics, no EHR, no alerts, just gut instinct and desperation. But here’s the twist: in India, we actually *know* the prices. We have to. We’ve learned to Google, to ask pharmacists, to barter. We don’t wait for the system to fix us-we fix ourselves. Maybe the U.S. doesn’t need more tech. Maybe it needs more grit. More desperation. More love for the patient sitting in front of you, not the algorithm behind the screen.
My cousin’s doctor in Mumbai wrote her a prescription for metformin and said, ‘Go to the pharmacy on the corner. Tell them Pooja sent you. They’ll give you 30 tablets for 20 rupees.’ No app. No pop-up. Just human connection. That’s what’s missing here.
We’ve turned healthcare into a transaction. But medicine? Medicine is a relationship. And relationships need honesty. Even when it’s hard.
Diana Stoyanova
January 21, 2026 AT 03:12Let me tell you something that keeps me up at night: I had a patient last week who came in with chest pain. Her ECG was fine, but her eyes were terrified. She whispered, ‘Doc, I’m not taking that pill. I can’t afford it.’ I asked how much. She said $180. I looked it up right then and there-it was $12 at CVS with a coupon. She started crying. Not from pain. From relief. From being seen.
That’s the moment I stopped being just a clinician. I became a translator. Between the system and the soul. Between the algorithm and the human.
And here’s the beautiful part-when you do this, it changes everything. You start asking, ‘What’s your budget?’ before you ask ‘What’s your symptom?’ You start learning the names of the pharmacies that offer discounts. You start teaching your residents to use GoodRx like they use UpToDate.
This isn’t about tech. It’s about courage. It’s about choosing to look at the price tag even when you know it’ll break your heart. Because if you don’t, you’re not healing. You’re just prescribing.
And if you’re not healing… what are you even doing here?
Micheal Murdoch
January 22, 2026 AT 22:57Just read the comment from Pooja in India. That’s the truth. We’re so busy trying to digitize compassion that we forgot how to be human. The tools are useless if we don’t use them with empathy. And empathy? That’s not in the EHR.