Drug Interaction Checker
Check Drug Interaction Risk
Two drugs taken together can save your life-or send you to the hospital. It’s not magic. It’s science. And the difference between pharmacokinetic and pharmacodynamic interactions determines how you manage that risk.
What’s the Difference Between PK and PD Interactions?
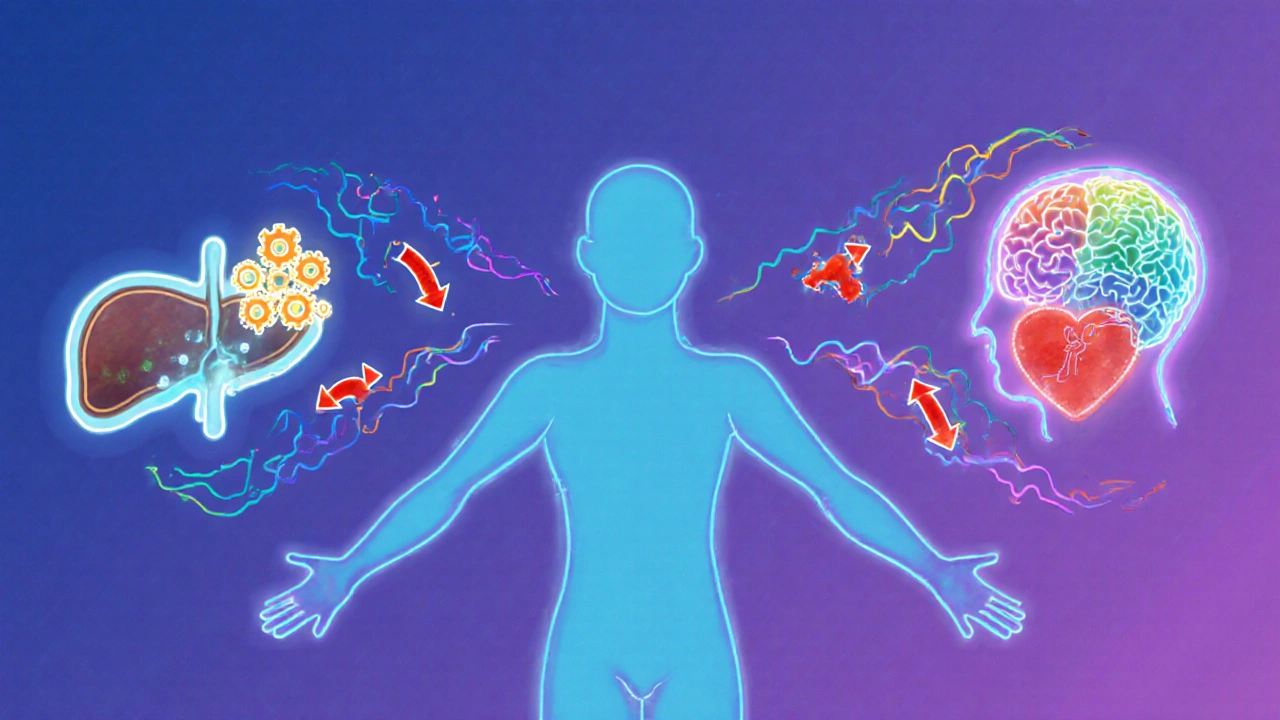
Think of pharmacokinetics (PK) as what your body does to the drug. That means absorption, distribution, metabolism, and excretion-collectively called ADME. If one drug changes how fast another is broken down or cleared from your system, that’s a PK interaction. Pharmacodynamics (PD) is what the drug does to your body. It’s about how the drug binds to receptors, triggers responses, or blocks other signals. When two drugs hit the same target-like both lowering blood pressure-you get a PD interaction. The key? PK changes the amount of drug at the site. PD changes the effect of that drug, even if the amount stays the same.How Pharmacokinetic Interactions Work
PK interactions are the most common reason for dangerous drug combos. About 47% of serious drug interactions fall into this category, according to Stockley’s Drug Interactions. Here’s how they happen:- Absorption: Antacids can cut absorption of antibiotics like ciprofloxacin by 75-90%. If you take Tums with your antibiotic, it won’t work.
- Distribution: Warfarin sticks to proteins in your blood. If you add phenylbutazone, it kicks warfarin off those proteins. Free warfarin levels jump 300%. That’s a bleeding risk.
- Metabolism: The liver uses enzymes-mainly CYP3A4, CYP2D6, and CYP2C9-to break down drugs. Clarithromycin (an antibiotic) blocks CYP3A4. If you’re on simvastatin (a statin), your body can’t clear it. Simvastatin levels spike 10-fold. Muscle damage? That’s real.
- Excretion: Probenecid slows down penicillin clearance by half. That’s why it was once used to boost penicillin’s effect.
These interactions don’t always show up right away. CYP3A4 inhibitors like clarithromycin take 3-5 days to reach full effect. That’s why people get caught off guard.
How Pharmacodynamic Interactions Work
PD interactions are sneakier. The drug levels look normal on a blood test-but the effect is wild. Three types:- Synergistic: The combo is stronger than the sum of its parts. Sildenafil (Viagra) + nitroglycerin = dangerous drop in blood pressure. This combo can kill.
- Additive: Effects stack. Warfarin + aspirin = higher bleeding risk. Both thin blood. Together, they’re worse.
- Antagonistic: One drug cancels the other. Naloxone blocks opioids. That’s how it reverses overdoses. But if you take an opioid painkiller with a drug that blocks its receptor, you’ll feel no pain relief.
PD interactions dominate in the brain. Eighty-five percent of CNS drug interactions-like mixing antidepressants and opioids-are pharmacodynamic. Serotonin syndrome from combining SSRIs and MAO inhibitors? That’s PD. No change in blood levels. Just a runaway chemical reaction.

Why Management Is Totally Different
You can’t treat PK and PD the same way. For PK interactions, you can often adjust the dose. If you need clarithromycin and simvastatin, drop the simvastatin to 10mg. Monitor liver enzymes. You’re still safe. For PD interactions? Often, you just avoid the combo. No dose tweak fixes it. MAO inhibitors and SSRIs? Never mix. The risk isn’t dose-dependent-it’s binary. One wrong combo, and you’re in ICU. Narrow therapeutic index drugs like warfarin, digoxin, and phenytoin are especially vulnerable to PK interactions. Sixty-eight percent of serious interactions with these drugs are pharmacokinetic. That’s why blood tests (TDM) are routine for these meds. PD interactions? They’re common with heart and brain meds. Fifty-two percent of cardiovascular interactions and 78% of CNS interactions are PD. That’s why doctors ask: “Are you taking anything for anxiety? Depression? Sleep?”Real-World Tools and Tech
Epic, Cerner, and other EHR systems now flag over 2,200 high-severity interactions. But they don’t always tell you why. Pharmacists are the frontline defense. A 2022 survey found pharmacist-led medication reviews cut adverse drug events by 42%. They don’t just check boxes-they ask: “Is this a PK or PD issue?” Therapeutic drug monitoring helps with PK. Target ranges exist for 37 drugs-from lithium to vancomycin. But PD? No blood test can catch serotonin syndrome before it hits. You need to watch symptoms: tremors, confusion, fever, fast heart rate. New tools are emerging. AI models now predict PD interactions with 89% accuracy-better than old rule-based systems. The FDA’s Sentinel Initiative found 17 new PD risks in 2022, including SGLT2 inhibitors (like dapagliflozin) combined with loop diuretics increasing dehydration risk by 2.3 times.
What You Should Do
If you’re on five or more meds (and 15% of adults over 65 are), here’s what to do:- Know your meds. Don’t just take them. Know why. Ask your pharmacist: “Is this combo safe?”
- Watch for timing. PK effects take days. PD effects can hit in minutes. If you feel dizzy, weak, or confused after starting a new drug, act fast.
- Don’t assume OTC is safe. St. John’s Wort blocks CYP3A4. It can tank your birth control or transplant meds.
- Use one pharmacy. They track everything. Chain pharmacies share data. Your local pharmacist sees the whole picture.
- Ask about alternatives. If you’re on simvastatin and need an antibiotic, ask if azithromycin (not clarithromycin) is an option. No CYP3A4 block.
The Bigger Picture
By 2030, better management of PK and PD interactions could prevent 1.3 million adverse events globally. That’s $28 billion saved. It’s not just about avoiding side effects. It’s about keeping people out of hospitals, out of ICUs, and alive. The science is clear. The tools are here. What’s missing is awareness. If you’re on multiple meds, don’t wait for a problem to happen. Ask the question now: “Could this combo be a PK or PD issue?”What’s the main difference between pharmacokinetic and pharmacodynamic interactions?
Pharmacokinetic (PK) interactions change how much drug reaches your system-by affecting absorption, metabolism, or excretion. Pharmacodynamic (PD) interactions change how your body responds to the drug, even if the amount stays the same. PK alters the dose-response curve horizontally; PD shifts it vertically.
Can you fix a pharmacokinetic interaction by changing the dose?
Yes, often you can. For example, if you need clarithromycin and are on simvastatin, reducing simvastatin to 10mg per day lowers the risk of muscle damage. Therapeutic drug monitoring helps guide these adjustments, especially for drugs like warfarin or digoxin.
Are pharmacodynamic interactions harder to detect than pharmacokinetic ones?
Yes. PK interactions show up in blood tests-you can see drug levels rise or fall. PD interactions don’t change concentrations. You have to watch symptoms: sudden dizziness, confusion, bleeding, or high blood pressure. That’s why they’re often missed until something serious happens.
Which drugs are most likely to cause dangerous interactions?
Narrow therapeutic index drugs like warfarin, digoxin, phenytoin, and lithium are high-risk for PK interactions. For PD, it’s CNS drugs (SSRIs, opioids, benzodiazepines), antihypertensives, and anticoagulants. Combining any two of these increases risk dramatically.
Can over-the-counter meds cause serious drug interactions?
Absolutely. St. John’s Wort blocks CYP3A4 and can reduce effectiveness of birth control, antidepressants, and transplant drugs. NSAIDs like ibuprofen can worsen kidney damage when taken with ACE inhibitors. Even common antacids can stop antibiotics from working. Always tell your pharmacist what you’re taking-even supplements.
How do electronic health records help with drug interactions?
Modern systems like Epic flag over 2,200 high-severity interactions-1,247 PK and 983 PD. But they don’t explain why. That’s why pharmacists are critical: they interpret the alerts, check for clinical relevance, and advise on alternatives. Alerts are a tool, not a replacement for expert judgment.
Is there a way to predict pharmacodynamic interactions before they happen?
Traditional methods rely on known receptor targets and clinical case reports. New AI models, like the one in Nature Medicine (2023), now predict PD interactions with 89% accuracy by analyzing drug structures and physiological pathways. But human expertise still leads-AI flags possibilities; clinicians confirm risks.






Jefriady Dahri
November 25, 2025 AT 05:53Man, this post is a lifesaver. I’ve been on 6 meds and didn’t even know St. John’s Wort could tank my birth control. My pharmacist just flagged it last week-glad I didn’t ignore it. Thanks for breaking it down like this. 🙌
Archana Jha
November 26, 2025 AT 21:48they dont want you to know this but the FDA and big pharma are hiding the real truth about pd interactions… its all about control and profits… they dont want you to know that your meds are designed to keep you sick so you keep buying… the cyp enzymes? totally manipulated by the shadow government… i saw it on a forum in 2017 and now its clear
Aki Jones
November 27, 2025 AT 08:44Let’s be real: PK and PD? That’s just corporate jargon to make you feel dumb while they sell you more pills. They don’t tell you that 80% of these ‘interactions’ are just statistical noise dressed up in lab coats. And don’t get me started on ‘therapeutic drug monitoring’-who’s paying for those tests? You are. And they’ll bill you for every single drop of blood they draw. It’s a racket. I’ve seen it. I’ve read the reports. And no, I’m not paranoid-I’m informed.
Dolapo Eniola
November 28, 2025 AT 06:02Bro, in Nigeria we don’t even have access to half these drugs, so why are you all stressing over PK/PD? We just take what’s available and pray. You Americans think too much. If your body doesn’t like it, you die. Simple. No fancy AI models needed. Just faith and a strong stomach. 😎
Sharley Agarwal
November 30, 2025 AT 05:25Typical. Another post pretending to educate while ignoring that 90% of these interactions are preventable with basic care. You people treat medicine like a video game-click the right combo, get the buff. Meanwhile, real people are dying because no one asked if they were taking turmeric with their blood thinner. Pathetic.
Andrew McAfee
December 2, 2025 AT 00:47Back home in Ghana, we used to mix herbs with Western meds without a second thought. No EHR, no pharmacist, no alerts. But we knew our bodies. We watched. We listened. We adapted. Maybe the real solution isn’t more tech-it’s trusting the human experience again. Not every interaction needs a database to be understood.
Andrew Camacho
December 3, 2025 AT 02:30Okay, but let’s be honest-this whole PK/PD thing is just a distraction. The real issue? Doctors don’t listen. They write scripts like they’re ordering coffee. I had a cardiologist prescribe me simvastatin AND clarithromycin and didn’t blink. I had to Google it myself. Then he acted like I was the problem. That’s not a drug interaction-that’s a systemic failure. And now I’m terrified to take anything. Thanks, healthcare.
Erika Hunt
December 3, 2025 AT 19:31I’ve been thinking about this a lot lately, especially since my mom started on five new medications after her stroke, and I’ve noticed that the more we try to quantify everything-enzyme pathways, blood levels, AI predictions-the more we forget that people aren’t data points. There’s something deeply human about watching someone’s face when they say, ‘I feel weird,’ and realizing that no algorithm can measure that kind of fear. Maybe the real breakthrough isn’t in predicting interactions, but in teaching doctors to pause, look up, and ask, ‘How are you really doing?’
Amy Hutchinson
December 5, 2025 AT 01:32You know what’s worse than drug interactions? People who don’t tell their doctors they’re taking CBD. I found out my neighbor’s husband had a seizure because he was on Keppra and started ‘natural anxiety relief’-no one knew. Just… don’t be that person. Tell them everything. Even the gummy vitamins.