
Getting your medication right isn’t just about taking it-it’s about taking it correctly, consistently, and on time. For people using inhalers, patches, or injectables, this is harder than it sounds. Studies show that between 30% and 70% of patients don’t take their medications as prescribed. That’s not laziness. It’s confusion, fear, frustration, or just plain forgetfulness. And it’s costing lives. In the U.S. alone, poor adherence leads to 125,000 preventable deaths every year and adds $100-289 billion to healthcare costs. The good news? There are real, proven ways to fix this-and they’re different for each type of medication.
Why Inhalers Are So Hard to Use Correctly
Inhalers look simple. You shake, puff, breathe in. But most people get it wrong. A 2022 study found that nearly 80% of asthma and COPD patients use their inhalers incorrectly. That means even if they take it every day, they’re not getting the full dose. The result? More flare-ups, more ER visits, more steroids in their system. The fix isn’t just telling patients to “do it better.” It’s showing them, step by step, with feedback. Electronic inhalers like Propeller Health’s sensor system attach to standard inhalers and record every puff. They sync to an app and tell you if you didn’t inhale deeply enough, or if you used it too fast. In one trial, patients using these devices improved their technique by 40% in just three months. That’s not magic-it’s real-time coaching. But tech alone doesn’t work. A pharmacist sitting with a patient, watching them use the inhaler, correcting their hand-breath timing, and then having them do it again-that’s what sticks. One study showed pharmacist-led training reduced hospitalizations by 28%. Combine that with the sensor data, and you’ve got a powerful combo.Patches: Discreet, But Problematic
Patches are supposed to be easy. Stick it on, forget about it. But skin irritation, peeling edges, and forgetting to change it make adherence shaky. A 2022 survey found that 31% of insulin patch users stopped using them because their skin got red or itchy. Others forgot to replace it every 3 days, or they’d stick it on a hairy area and it wouldn’t stick. Newer patches are better. Some now come with built-in sensors that detect if the patch is still on the skin. Proteus Digital Health’s ingestible sensor, approved by the FDA in 2023, goes even further. It’s swallowed with the patch and activates in the stomach, sending a signal that the medication was taken. It doesn’t track skin contact, but it confirms ingestion-something no patch ever could before. Still, the simplest fix is often the best: reminders. A text message or app alert saying, “Time to change your patch,” works better than you’d think. One study showed a 22% increase in adherence with daily reminders. And for older adults, having a caregiver help with patch changes-not just remind, but actually do it-makes a huge difference.Injectables: More Than Just a Shot
Injectables like insulin, biologics for rheumatoid arthritis, or monthly migraine treatments require more than just sticking a needle in. They need precision. Too much? Too little? Wrong time? All bad. That’s where smart pens come in. Novo Nordisk’s connected insulin pens track the exact time, dose, and location of every injection. They sync to an app and show patterns-like if you’re always skipping your evening dose because you’re too tired. Users report a 27% improvement in dose accuracy. But here’s the catch: 22% of older users said the app was too complicated. That’s why the best systems don’t just send data-they simplify it. A simple green light on the pen says “Dose logged.” No app needed. For caregivers, a weekly email summary works better than a dashboard full of graphs. Another big win? Extended-release formulas. Instead of daily injections, some medications now come in monthly or even quarterly doses. That cuts down the mental load. For people on long-term treatments, fewer injections mean fewer reasons to skip. One study showed a 25% improvement in adherence with extended-release versions compared to daily shots.
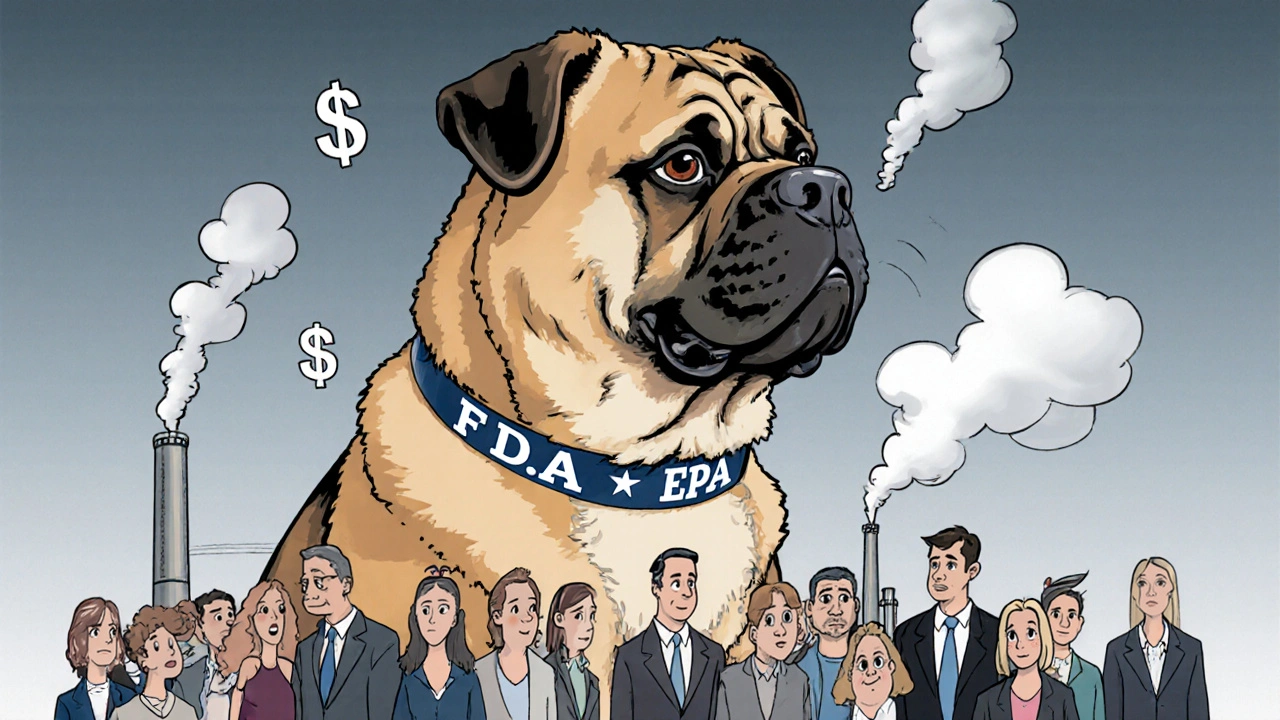
The Five Dimensions of Adherence
Doctors and pharmacists used to think adherence was about remembering. It’s not. Dr. Richard B. Martinello from Yale says there are five real barriers: affordability, accessibility, acceptability, awareness, and activation. - Affordability: Is the medication too expensive? If you have to choose between your inhaler and groceries, you’ll skip it. - Accessibility: Can you get it? Do you have transportation? Is the pharmacy open when you’re off work? - Acceptability: Do you hate the side effects? Do you feel embarrassed using an inhaler in public? Do you fear needles? - Awareness: Do you even know how to use it right? Most people don’t. - Activation: Do you feel in control? Or like you’re just following orders? The most effective programs don’t just hand out devices. They ask: “What’s making this hard for you?” Then they fix that. One patient skipped patches because they were itchy. The pharmacist switched them to a different adhesive. Another couldn’t afford their insulin. The clinic connected them with a patient assistance program. These aren’t tech solutions-they’re human ones.What Works Best: Tech, Training, or Both?
Let’s be clear: gadgets help, but they’re not the whole answer. A smart inhaler that tracks your puffs is useless if you don’t know how to use it. A connected pen won’t help if you’re scared of needles. The best results come from combining two things: education and technology. - Start with a simple tool like the 8-item Morisky Scale to find out where the gaps are. Are you forgetting? Confused? Afraid? - Then match the solution. If it’s forgetfulness, use reminders. If it’s technique, use video coaching. If it’s cost, connect with support programs. - Follow up. Not once. Not at the pharmacy. Monthly for the first three months. That’s when habits form. Studies show that patients who get this kind of structured support have 37% better long-term adherence than those who just get a one-time lecture.Real People, Real Stories
On Reddit, a user named u/BreathEasy99 said their Propeller sensor boosted their inhaler use from 55% to 82% in three months. But they also said the app crashed twice a week on their Android phone. Another user, u/WheezyWarrior, stopped using their smart inhaler because the constant reminders made them anxious. These aren’t bugs. They’re design flaws. If your tech makes people feel watched, judged, or frustrated, it backfires. The same goes for patches. One patient said they loved the discretion-no one could tell they were on medication. But when the patch peeled off during a shower, they felt guilty. They didn’t tell their doctor. They just stopped. The lesson? Technology must be forgiving. It should say, “You missed one. That’s okay. Try again tomorrow.” Not, “You failed.”
What’s Coming Next
The market for adherence tech is exploding. It hit $2.8 billion in 2022 and could hit $8.5 billion by 2028. Propeller Health just launched AI that predicts when you’re likely to skip a dose-48 hours ahead. Novartis and GSK are spending hundreds of millions on this. By 2027, 75% of inhalers will have built-in tracking. But here’s the catch: only 37% of private insurance plans in the U.S. cover these devices. Medicare Advantage improved from 12% to 29% coverage between 2020 and 2023, but that’s still not enough. If you can’t afford the sensor, you can’t use it. The future isn’t just smarter devices. It’s fairer access. It’s making these tools available to everyone-not just the tech-savvy or well-insured.What You Can Do Today
You don’t need a smart inhaler to improve adherence. Start here:- Ask your pharmacist to watch you use your inhaler or injectable. Do it in person. No excuses.
- Set a daily phone alarm labeled with your medication name-not just “Med Time.”
- If patches peel off, try a different brand or use medical tape to secure the edges.
- Keep a simple log: “Took my shot? Yes/No.” Just writing it down helps.
- Ask if your medication has a long-acting version. One shot a month beats seven a week.
- Don’t be ashamed to say, “I’m struggling.” Your doctor can’t help if they don’t know.
Why do people stop using inhalers even when they know they need them?
Many stop because they don’t use them correctly and don’t feel the benefit. Others feel embarrassed using them in public, or find the side effects (like hoarseness or oral thrush) unpleasant. Some think they’re fine when symptoms disappear and stop taking it-never realizing the inhaler is preventing flare-ups, not just treating them. Without proper coaching, they assume the medication isn’t working.
Can smart patches really tell if I took my medication?
Some newer patches have sensors that detect if they’re still on your skin, but they can’t confirm the drug entered your body. The only patch system that confirms ingestion is Proteus Digital Health’s, which uses a tiny sensor you swallow with the patch. It activates in your stomach and sends a signal to your phone. But it’s not yet widely available and requires a prescription. Most “smart” patches only track skin contact, which isn’t the same as adherence.
Are connected insulin pens worth the cost?
For people who struggle with dose accuracy or forget injections, yes. Studies show a 27% improvement in correct dosing. For caregivers managing someone else’s insulin, the weekly summaries reduce errors. But if you’re already consistent and don’t need data, the $100-300 annual cost may not be worth it. Ask your doctor if your insurance covers it-some Medicare Advantage plans do now.
What’s the cheapest way to improve adherence?
Talk to your pharmacist. Many offer free, 10-15 minute sessions to check your technique. Use a simple pillbox or calendar to mark doses. Set phone reminders with the medication name. These cost nothing and can improve adherence by 20-30%. The most powerful tool isn’t a device-it’s a conversation.
Do electronic reminders actually work for long-term use?
They work well for the first 3-6 months, but many people turn them off after that. Why? Too many alerts feel nagging. Others forget to charge the device. The key is personalization: one alert per day, not five. And pairing it with a human check-in-like a nurse calling every two weeks-makes it stick longer. Tech is a helper, not a replacement for support.
Is there a difference between adherence and compliance?
Yes. Compliance means following orders. Adherence means you’re actively engaged in your care. Someone compliant takes their pill because they were told to. Someone adherent understands why it matters and chooses to do it-even when they don’t feel like it. Modern medicine focuses on adherence because it leads to better outcomes and fewer side effects from rushed or missed doses.




Tony Du bled
December 22, 2025 AT 00:39Man, I’ve been on an inhaler for years and never knew 80% of people mess up the technique. I thought I was doing it right until my pharmacist sat me down and showed me I was puffing like a dragon with a cold. Now I use the app. It’s not perfect, but at least I know when I screw up. No more guessing.
Kathryn Weymouth
December 23, 2025 AT 00:00The distinction between compliance and adherence is critical and often overlooked in clinical literature. Adherence implies agency, autonomy, and understanding-factors that are foundational to sustainable health behavior. The emphasis on human interaction over technological surveillance reflects a paradigm shift toward patient-centered care, which is not merely preferable but ethically imperative.
Herman Rousseau
December 23, 2025 AT 15:46Biggest win? Talking to your pharmacist. Seriously. No fancy app, no smart patch-just a 10-minute chat. I used to skip my patches because they itched. My pharmacist switched me to a different brand, gave me tape to hold it down, and asked if I was stressed. Turns out I was. Now I use it every time. No tech needed. Just a person who listens.
Candy Cotton
December 24, 2025 AT 09:31This article is a disgrace to American medical standards. We have the most advanced technology on Earth, yet we allow patients to fail because of ‘affordability’ and ‘acceptability’? This is not healthcare-it’s social work disguised as medicine. If you can’t afford your medication, you shouldn’t be taking it. The system must be held accountable, not the patient.
Gabriella da Silva Mendes
December 24, 2025 AT 11:23Okay but let’s be real-how many of these ‘smart’ devices are just expensive toys for rich people who already have their shit together? I work two jobs, my phone dies by 3 PM, and I’m supposed to care about an app that pings me 17 times a day? And don’t get me started on the patches that peel off in the shower. I’m not a lab rat. I’m a human who just wants to feel okay without being monitored like a criminal. 😒
Kiranjit Kaur
December 24, 2025 AT 11:25Love how this talks about human connection over tech. In India, we don’t have smart inhalers everywhere, but we have aunties who check in. My grandma’s neighbor reminds her to take her insulin every morning with chai. No app. Just care. Maybe the future isn’t AI-it’s community. ❤️
Sai Keerthan Reddy Proddatoori
December 24, 2025 AT 21:08Smart patches? Sensors? This is all part of the Big Pharma surveillance agenda. They want to track your every move, then charge you more. The government is in on it. They don’t care if you live or die-they care about data. You think your insulin pen is helping you? It’s feeding your info to the corporations. Wake up.
Sam Black
December 26, 2025 AT 16:28I’ve spent years watching people struggle with these devices. The real tragedy isn’t the tech-it’s that we treat adherence like a moral failing. It’s not. It’s a design flaw. If your system makes someone feel ashamed, you’ve already lost. The best innovation isn’t a sensor-it’s a quiet moment where someone says, ‘I’ve been there too.’
Julie Chavassieux
December 26, 2025 AT 19:14So... you're telling me... that... people... don't... take... their... meds... because... they're... scared?... or... broke?... or... just... tired?... Like... wow...
Vikrant Sura
December 28, 2025 AT 10:3437% adherence improvement with structured support? That’s statistically significant but clinically irrelevant. Most patients still fail. The data is cherry-picked. Real-world adherence is closer to 20%. And those ‘smart pens’? They’re overpriced garbage that breaks after six months. Don’t fall for the hype.
Jeremy Hendriks
December 29, 2025 AT 14:29Adherence isn’t about willpower. It’s about power. Who holds the power? The doctor? The algorithm? The insurance company? We’re told to ‘take responsibility,’ but we’re never given the tools to actually do it. The system isn’t broken-it’s designed to make you fail. And then it sells you the fix.
Tarun Sharma
December 31, 2025 AT 05:14Simple reminder systems remain the most effective low-cost intervention. Pharmacist-led instruction is underutilized. Cost-effective, scalable, and human-centered. Recommend implementation in all primary care settings.
Aliyu Sani
January 1, 2026 AT 06:27yo the whole smart patch thing is wild but like… if your body dont absorb the drug even if the sensor says u took it… then u still ain’t good. the tech is cool but it dont fix the real issue: people dont got access to good docs. i seen folks in Lagos take their meds but the meds be expired. no sensor gonna fix that.