Cholesterol Medication Decision Guide
Find Your Best Cholesterol Medication
This tool helps you understand which cholesterol medication might be most suitable for your specific situation based on factors like LDL levels, side effects, and other medications.
High cholesterol isn’t just a number on a lab report-it’s a silent risk that can lead to heart attacks or strokes. If you’ve been prescribed Zocor (simvastatin), you’re not alone. Millions use it to lower LDL, the "bad" cholesterol. But maybe your doctor mentioned alternatives. Or maybe you’re experiencing side effects. Or perhaps you’re wondering if there’s something better. This isn’t about switching for the sake of change. It’s about finding the right fit for your body, lifestyle, and health goals.
What Zocor (Simvastatin) Actually Does
Zocor is the brand name for simvastatin, a statin drug first approved in the 1990s. It works by blocking an enzyme in your liver called HMG-CoA reductase. That enzyme is responsible for making cholesterol. When it’s slowed down, your liver pulls more LDL out of your bloodstream. Simple. Effective. But not perfect for everyone.
Typical starting doses range from 5 mg to 20 mg daily, taken in the evening-when your liver is most active in cholesterol production. Most people see a 30% to 40% drop in LDL cholesterol within 4 to 6 weeks. For someone with an LDL of 180 mg/dL, that could mean dropping to 110 mg/dL or lower. That’s a meaningful change.
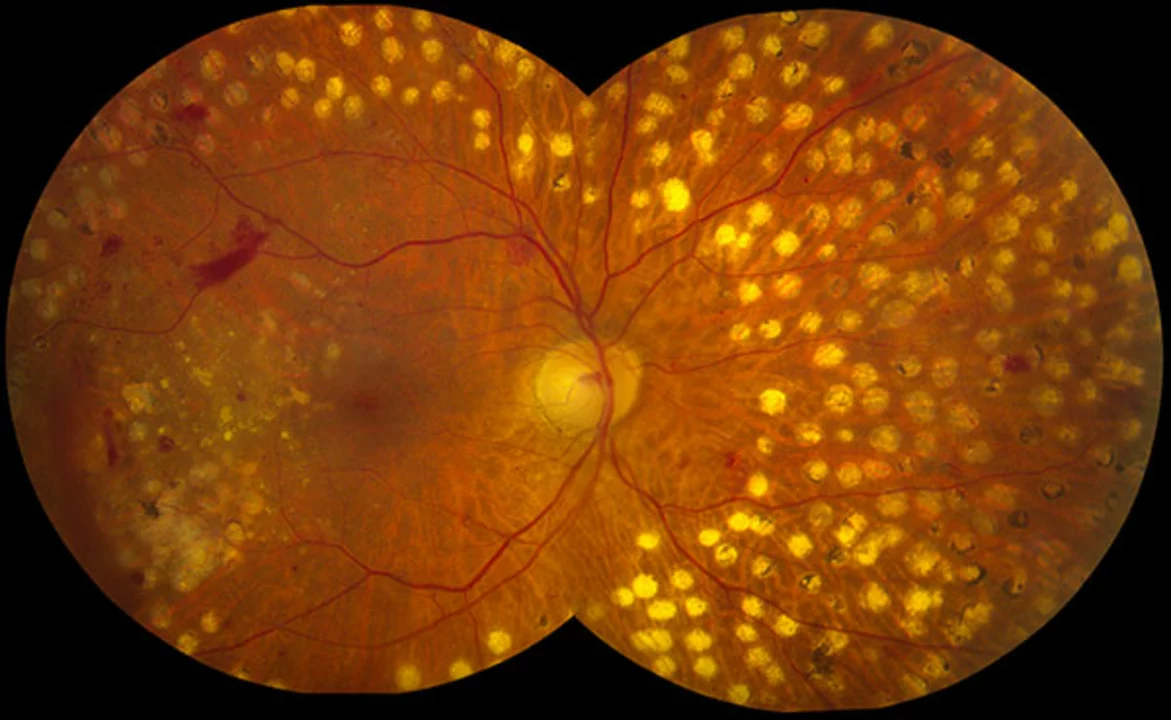
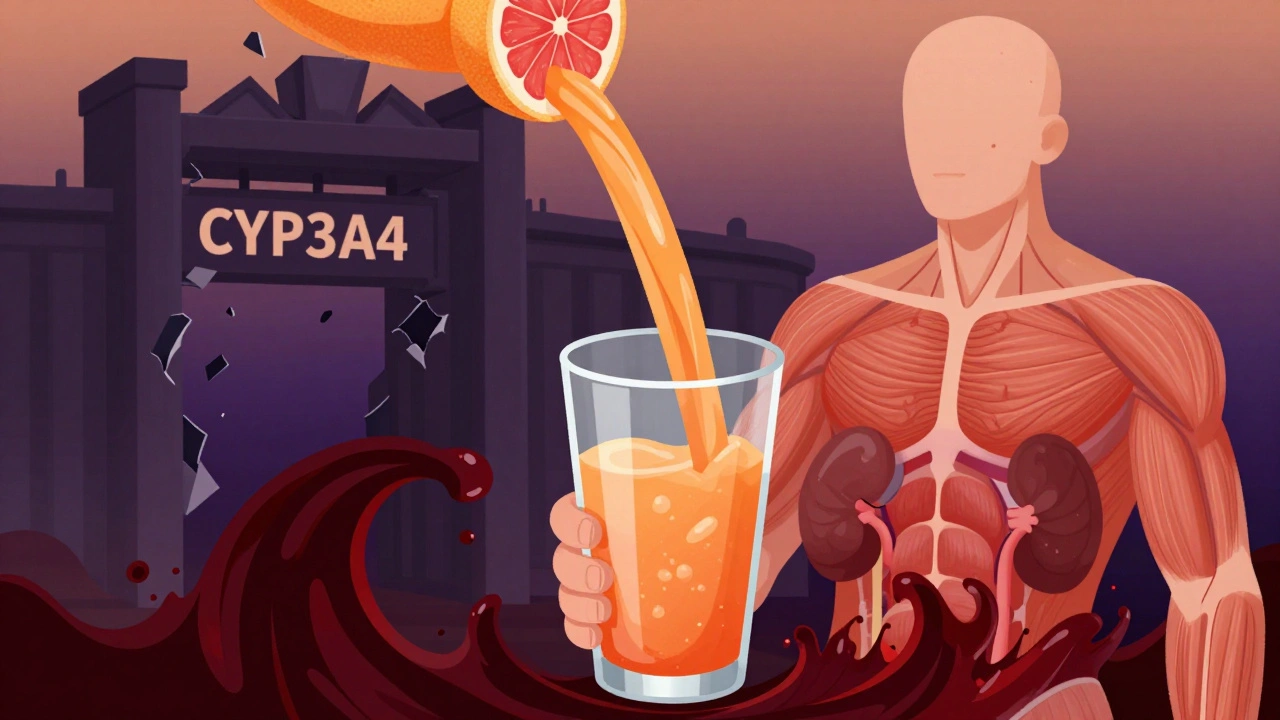
But here’s the catch: not everyone tolerates it. Muscle pain, fatigue, and elevated liver enzymes are the most common complaints. In rare cases, a serious condition called rhabdomyolysis can occur, especially when simvastatin is taken with certain other drugs like fibrates or grapefruit juice. That’s why some people look at alternatives.
Atorvastatin (Lipitor): The Stronger Statin
If simvastatin isn’t cutting it-or if you need a bigger drop in cholesterol-atorvastatin (Lipitor) is often the next step. It’s more potent. A 10 mg dose of atorvastatin lowers LDL about as much as a 20 mg dose of simvastatin. At 40 mg or 80 mg, it can reduce LDL by 50% or more.
That makes it ideal for people with very high cholesterol, familial hypercholesterolemia, or those who’ve already had a heart attack. Studies show atorvastatin reduces cardiovascular events more than simvastatin at equivalent doses. It also has a longer half-life, so timing doesn’t matter as much-you can take it anytime of day.
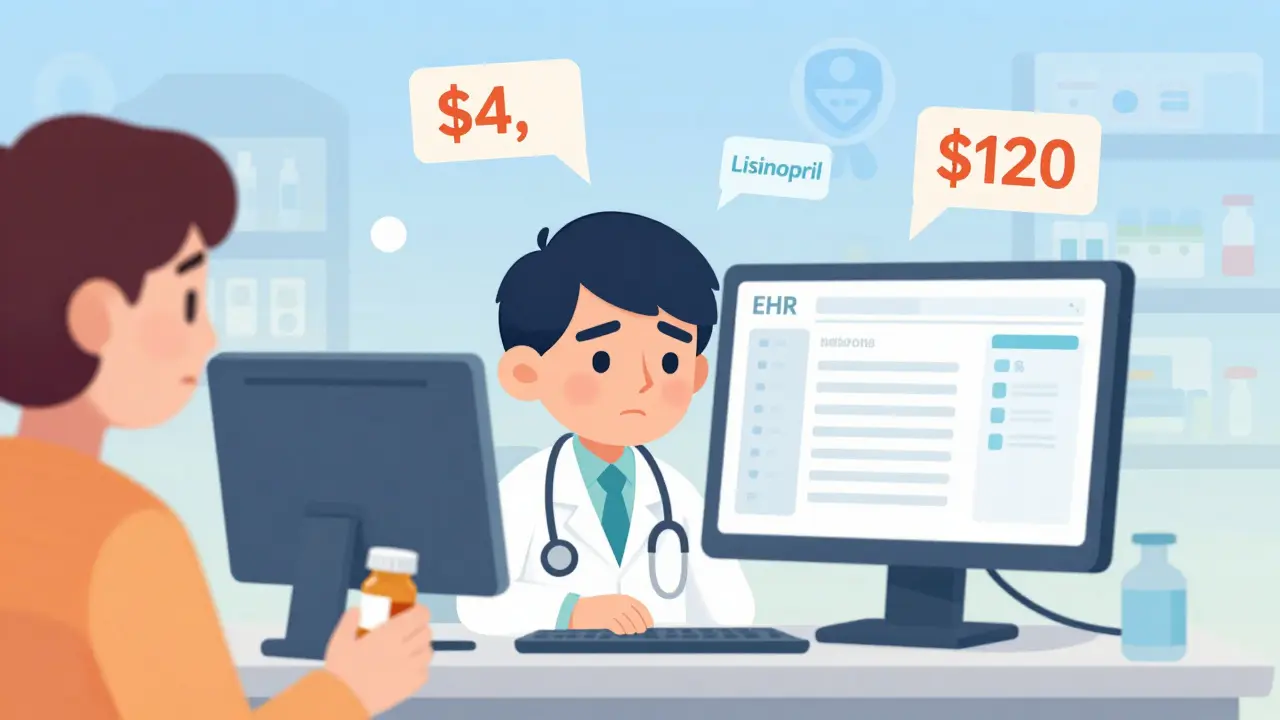
But stronger doesn’t always mean better. Higher doses of atorvastatin carry a slightly higher risk of muscle issues and new-onset diabetes. It’s also more expensive than generic simvastatin. If your LDL is just moderately high and you’re doing well on 20 mg of simvastatin, switching might not be worth it.
Rosuvastatin (Crestor): The Fast-Acting Option
Rosuvastatin (Crestor) is another potent statin. It’s the most powerful in its class for lowering LDL-up to 55% reduction at 20 mg. It also raises HDL (the "good" cholesterol) a bit more than simvastatin. Rosuvastatin is often chosen for people who need fast, significant results.
One advantage: it’s less likely to interact with other medications. Unlike simvastatin, it’s not broken down by the same liver enzyme (CYP3A4), so it’s safer if you’re on other drugs like blood pressure meds or antibiotics. It’s also cleared mostly by the kidneys, so if you have liver issues, it might be a better fit.
But it’s not without trade-offs. Rosuvastatin has a higher risk of muscle toxicity in people of Asian descent, and it’s more likely to cause protein in the urine. It’s also pricier. For many, it’s a good option-but only if you need that extra punch.
Pravastatin: The Gentle Statin
If muscle pain is your main concern with simvastatin, pravastatin might be the answer. It’s one of the mildest statins. It doesn’t rely heavily on the CYP3A4 liver enzyme, so drug interactions are rare. It’s also less likely to cause muscle aches or liver enzyme spikes.
But it’s weaker. A 40 mg dose of pravastatin lowers LDL by only about 25% to 30%. That’s fine if your cholesterol is borderline high and you’re mostly focused on prevention. But if your LDL is above 190 mg/dL, you’ll likely need something stronger.
Pravastatin is also the only statin that doesn’t cross the blood-brain barrier, which some researchers believe might reduce rare neurological side effects. If you’re older, on multiple medications, or sensitive to drugs, it’s a smart, low-risk choice.
Non-Statin Alternatives: When Statins Aren’t Enough
Some people can’t take statins at all. Others need more than a statin alone. That’s where non-statin options come in.
Ezetimibe (Zetia) works differently. Instead of blocking cholesterol production, it blocks cholesterol absorption in your gut. It’s usually added to a statin, not used alone. Alone, it lowers LDL by about 15% to 20%. But when paired with simvastatin (as Vytorin), it can push LDL down another 20% or more. Side effects are mild-mostly stomach upset.
PCSK9 inhibitors like evolocumab (Repatha) and alirocumab (Praluent) are injectables. They’re for people with very high cholesterol or genetic conditions like familial hypercholesterolemia. They can drop LDL by 60% or more. But they cost over $14,000 a year. Insurance often requires you to fail two statins before approving them.
Bempedoic acid (Nexletol) is newer. It works in the liver like a statin but in a different spot, so it’s less likely to cause muscle pain. It lowers LDL by about 20% and is often used with ezetimibe. It’s taken as a pill once a day. It’s not as powerful as high-dose statins, but it’s a solid option for statin-intolerant patients.
How to Decide What’s Right for You
There’s no one-size-fits-all. Here’s how to think about it:
- How high is your LDL? Above 190? You likely need a strong statin like atorvastatin or rosuvastatin. Below 160? Simvastatin or pravastatin may be enough.
- Have you had a heart event? If you’ve had a heart attack or stroke, you need aggressive treatment. Atorvastatin or rosuvastatin at higher doses are preferred.
- Are you taking other meds? If you’re on antibiotics, antifungals, or blood thinners, avoid simvastatin. Pravastatin or rosuvastatin are safer.
- Do you get muscle pain? Try switching to pravastatin or bempedoic acid. If it stops, you’ve found your match.
- What’s your budget? Simvastatin and pravastatin cost under $10 a month as generics. Rosuvastatin and atorvastatin are more expensive. PCSK9 inhibitors? You’ll need insurance approval.
Many people start with simvastatin because it’s cheap and effective. But if you’re not hitting your target LDL after 8 weeks, or you’re having side effects, don’t just tough it out. Talk to your doctor about switching or adding another medication.

Real-World Outcomes: What Works Best?
A 2023 analysis of over 2 million patients in the U.S. and Europe found that people on atorvastatin or rosuvastatin had a 15% lower risk of heart attack than those on simvastatin, even after adjusting for age and other risk factors. But the difference in death rates was small. That’s important: lowering cholesterol doesn’t always mean living longer-but it does mean fewer heart attacks.
Another study showed that 1 in 4 people on simvastatin stopped taking it within a year because of side effects. The same study found that switching to pravastatin or ezetimibe helped 70% of those people stay on treatment.
It’s not about which drug is "best." It’s about which one you can take consistently. The best cholesterol medicine is the one you don’t quit.
What to Do Next
If you’re on Zocor and doing fine-no side effects, LDL under 100 mg/dL-stick with it. Don’t fix what isn’t broken.
If you’re struggling with side effects, write down what you’re feeling: muscle soreness? Fatigue? Trouble sleeping? Bring that list to your doctor. Don’t guess. Don’t stop cold turkey. Statins need to be tapered or switched carefully.
If your LDL is still too high after 3 months, ask about adding ezetimibe. It’s safe, cheap, and works well with statins. If you’re still not there, discuss bempedoic acid or a higher-potency statin.
And if you’re unsure? Get a lipid panel done. Know your numbers. Know your options. Cholesterol management isn’t a one-time decision. It’s an ongoing conversation with your health.
Is simvastatin the same as Zocor?
Yes. Zocor is the brand name for simvastatin. The active ingredient is identical. Generic simvastatin works the same way and costs far less.
Can I switch from Zocor to Lipitor on my own?
No. Switching statins requires medical supervision. Doses aren’t directly interchangeable. Atorvastatin is stronger, so switching without adjusting the dose could lead to too much or too little medication. Always consult your doctor before changing.
Which statin has the least side effects?
Pravastatin and fluvastatin tend to have the lowest rates of muscle-related side effects. Rosuvastatin and atorvastatin are more potent but carry slightly higher risks. The "least side effects" depends on your genetics, other medications, and health history.
Is there a natural alternative to Zocor?
Red yeast rice contains a compound similar to statins and can lower LDL by 15% to 25%. But it’s not regulated like prescription drugs-potency and safety vary. Some batches contain toxic contaminants. It’s not recommended as a replacement without medical oversight.
How long does it take for a new cholesterol medication to work?
Most statins and ezetimibe start working within a week, but it takes 4 to 6 weeks to reach full effect. Your doctor will usually check your cholesterol levels after 6 to 8 weeks to see if the dose or drug needs adjusting.
What If Nothing Seems to Work?
If you’ve tried multiple statins, ezetimibe, and bempedoic acid-and your LDL is still above 130 mg/dL-you might have familial hypercholesterolemia. That’s a genetic condition where your body makes too much cholesterol no matter what you eat or do.
In those cases, PCSK9 inhibitors are often the answer. They’re injectables given every two to four weeks. They’re not cheap, but for people at high risk, they’re life-saving. Some insurance plans now cover them after one statin fails, not two.
Don’t give up. There’s almost always another option. The goal isn’t perfection. It’s progress. Lowering LDL by even 20% can cut your heart attack risk in half. Every percentage point counts.



Aditya Singh
October 30, 2025 AT 13:14Let’s be real-simvastatin is the pharmaceutical equivalent of a 2005 Honda Civic: reliable, cheap, and universally available, but it’s not gonna win any races. Atorvastatin? That’s the Tesla Model S. Higher potency, longer half-life, superior lipid modulation via HMG-CoA reductase inhibition with pleiotropic effects on endothelial function and CRP reduction. Rosuvastatin? Even more potent, with superior LDL-C reduction (up to 55%) and HDL-C elevation via ABCA1 upregulation. But here’s the kicker-pharmacogenomics. CYP3A4 polymorphisms in South Asian populations significantly increase simvastatin exposure, leading to higher myopathy risk. So yeah, switching to rosuvastatin or pravastatin isn’t just clinical-it’s personalized medicine 101.
Katherine Reinarz
November 1, 2025 AT 10:40ok so i switched from zocor to lipitor and like?? my legs felt like jelly and i was so tired i napped at my desk and my boss thought i was dead?? like?? why does this stuff make you feel like a zombie?? also i ate grapefruit once and now i’m scared of citrus??
John Kane
November 3, 2025 AT 00:49Hey everyone, I just want to say how much I appreciate this thread-it’s rare to see such thoughtful, real talk about something as personal as cholesterol management. I’ve been on pravastatin for three years now after my first statin gave me muscle cramps so bad I couldn’t walk the dog. Switching wasn’t easy, but finding the right fit? That’s the real win. And if you’re worried about cost, remember: generics are lifesavers. Simvastatin costs less than a cup of coffee a day. But more than that-it’s about listening to your body. If something feels off, speak up. Your doctor isn’t a robot, and you’re not just a number. You’re a person trying to live well. Keep asking questions. Keep showing up. You’ve got this.
Callum Breden
November 4, 2025 AT 15:28It is frankly irresponsible to suggest that patients consider switching statins without comprehensive lipid profiling, hepatic enzyme monitoring, and genetic screening for SLCO1B1 polymorphisms. The casual tone of this article betrays a dangerous oversimplification of a complex pharmacological landscape. Simvastatin’s association with rhabdomyolysis is not a mere "catch"-it is a clinically significant, potentially fatal adverse event. To recommend ezetimibe as a "safe" adjunct without addressing its modest efficacy and lack of mortality benefit is misleading at best. This is not health advice-it is wellness content masquerading as medical guidance.
Mansi Gupta
November 5, 2025 AT 03:27Thank you for writing this. I’ve been on simvastatin for five years and never questioned it until my LDL stayed stubbornly high. Switching to pravastatin made a difference-not because it was "better," but because my body finally tolerated it. I think the most important thing is consistency. I’ve seen too many people quit because of side effects or fear, then end up in the ER. It’s okay to need help. It’s okay to try different things. You’re not failing-you’re learning.
Erin Corcoran
November 6, 2025 AT 09:43OMG YES to the grapefruit warning!! 😱 I didn’t know it could mess with statins and I was chugging it every morning… now I’m paranoid about every fruit 😅 Also-ezetimibe is a total game changer when paired with a statin! My doc added it and my LDL dropped another 25% with zero side effects. So simple, so cheap. Why isn’t everyone doing this??
shivam mishra
November 6, 2025 AT 18:30As a pharmacist in Mumbai, I see this every day. People stop simvastatin because of muscle pain and then buy red yeast rice online because it’s "natural." Big mistake. Those supplements aren’t regulated-some batches have lovastatin at uncontrolled doses and heavy metal contamination. I’ve seen three cases of acute kidney injury from it. If you can’t tolerate statins, talk to your doctor about bempedoic acid. It’s not magic, but it’s safer than random internet pills. And yes, pravastatin is the gentlest. Many of my elderly patients do great on it. No CYP3A4 drama. Just steady, quiet results.
Scott Dill
November 6, 2025 AT 19:28Wait-so if I’m on Zocor and my LDL is 110 and I feel great, I shouldn’t switch? Like… at all? Even if my friend’s cousin’s yoga teacher said Lipitor is the future? I’m just trying to figure out if I’m overthinking this. I mean, I don’t want to be the guy who stops taking his meds because he saw a TikTok.
Arrieta Larsen
November 8, 2025 AT 16:07I’ve been on rosuvastatin for two years. My LDL dropped from 210 to 85. I take it at night. No muscle pain. No fatigue. But I did notice increased urination at first-turned out I had microalbuminuria, which my doctor caught early because of the test. So yes, it’s powerful. But also, get checked. Don’t assume it’s fine just because you feel okay.
Mike Gordon
November 8, 2025 AT 21:52