
BPH Anticholinergic Risk Calculator
Calculate Your Risk
Enter your BPH diagnostic metrics below. Based on FDA and AUA guidelines, this tool helps determine if anticholinergics like Vesicare or Detrol are safe for you.
Men over 65 with an enlarged prostate are often prescribed anticholinergics to control sudden urges to urinate. But for many, these drugs don’t just help-they can lock the bladder shut. If you or someone you know has benign prostatic hyperplasia (BPH) and is on oxybutynin, solifenacin, or tolterodine, this isn’t just a side effect warning. It’s a real, documented danger that sends thousands to the emergency room every year.
How Anticholinergics Work-and Why They’re Dangerous for Prostate Patients
Anticholinergics like Vesicare, Detrol, and Toviaz block a chemical in your body called acetylcholine. This chemical tells your bladder muscle to squeeze and empty. For someone with an overactive bladder, that’s helpful. But if your prostate is enlarged and already squeezing your urethra shut, your bladder is already working overtime just to push urine out. Adding an anticholinergic is like turning down the engine on a car stuck in mud. It doesn’t fix the blockage-it makes it worse.
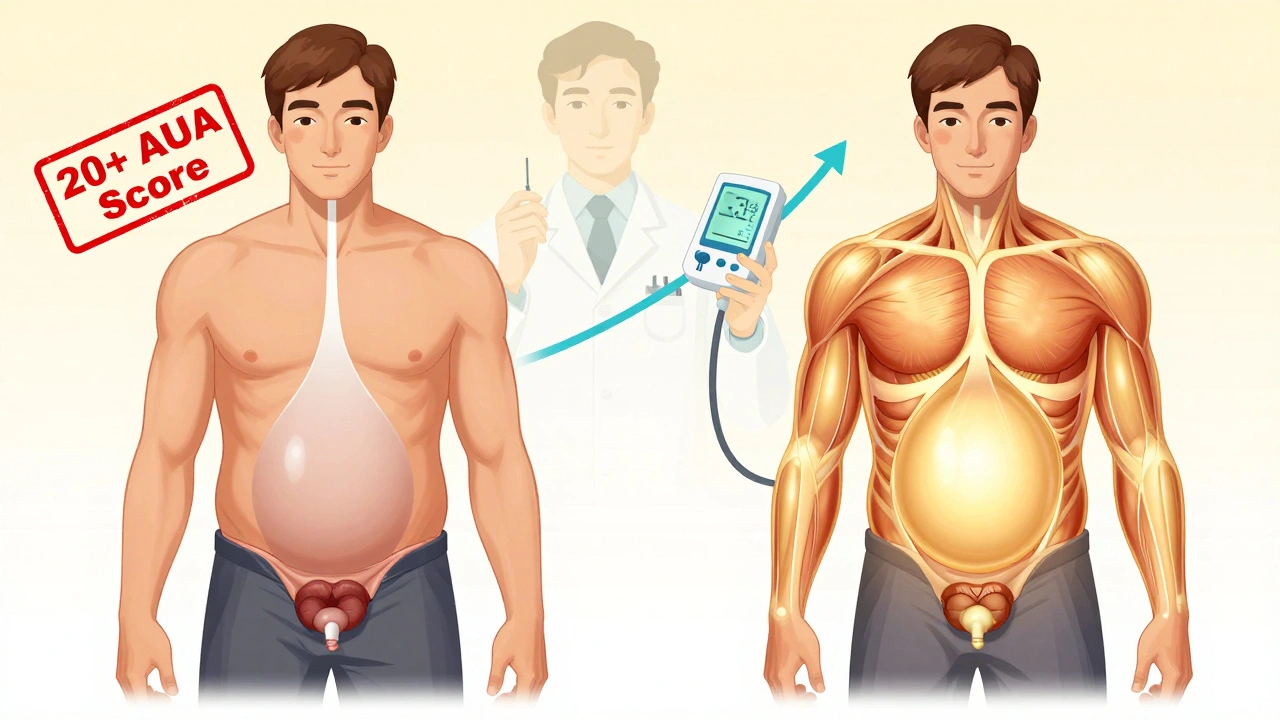
Studies show these drugs reduce urinary frequency by about one episode every two days. Sounds small? That’s because it is. The number needed to treat-how many people you have to give the drug to see one person benefit-is seven. Meanwhile, 8 to 15% of users report trouble urinating. In men with BPH, that risk jumps to over 20%. And for some, it leads to complete urinary retention: a bladder swollen with over a liter of urine, pain, and an emergency catheter.
The Double Hit: BPH + Anticholinergics = High Risk
Benign prostatic hyperplasia isn’t just about a bigger prostate. It’s about your bladder adapting to constant obstruction. The detrusor muscle-the main bladder muscle-gets thicker, stronger, and stretched thin trying to push urine past the blockage. When you add an anticholinergic, you’re weakening that muscle right when it needs to be at its strongest. That’s the double hit.
A 2020 review in Australian Prescriber found that men with BPH who take anticholinergics have a 2.3 times higher risk of acute urinary retention than those who don’t. The American Urological Association (AUA) updated its guidelines in 2018 to say: avoid anticholinergics in men with AUA symptom scores above 20 or prostate volumes over 30 grams. That’s not a suggestion-it’s a red flag.
One study tracked 142 men with BPH on online forums. Seventy-eight percent reported negative experiences. Thirty-four percent ended up with a catheter. One man, posting on Reddit under ‘BPHWarrior,’ said his Detrol prescription led to a 1,200 mL bladder, ER visit, and permanent catheter. He’s now facing surgery. These aren’t rare cases. Between 2018 and 2022, the FDA recorded 1,247 cases of urinary retention tied to anticholinergics. Sixty-three percent involved men over 65 with diagnosed BPH.
What Alternatives Actually Work?
If anticholinergics are risky, what’s left? There are safer, proven options.
Alpha-blockers like tamsulosin (Flomax) and alfuzosin (Uroxatral) relax the muscles around the prostate and bladder neck. They don’t touch the bladder’s squeezing power-they just make it easier for urine to flow. A 2008 review in American Family Physician showed men with BPH who started alpha-blockers right after catheter removal had a 30-50% higher chance of successfully voiding within 2-3 days than those on placebo.
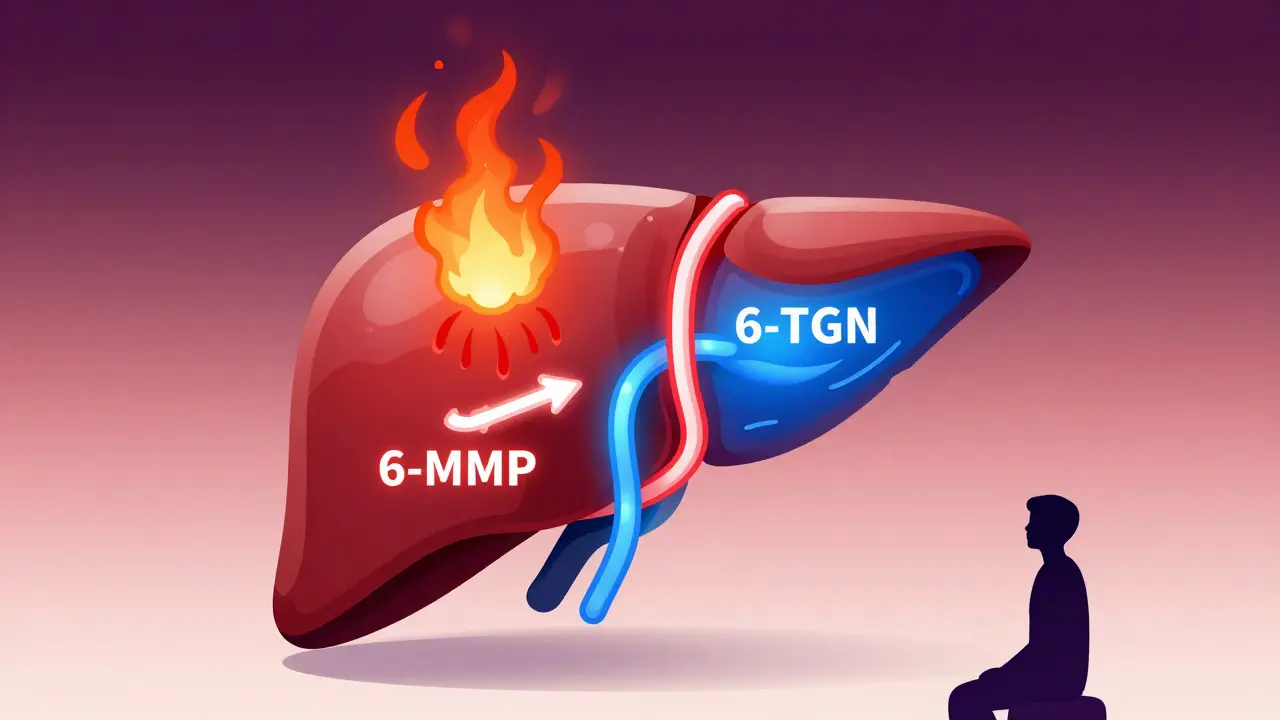
5-alpha reductase inhibitors like finasteride (Proscar) and dutasteride (Avodart) shrink the prostate over time. They take months to work, but long-term use cuts the risk of acute retention by half. They’re not for sudden relief-but they’re for long-term safety.
And then there’s mirabegron (Myrbetriq) and vibegron (Gemtesa). These are beta-3 agonists. Instead of blocking bladder contractions, they gently stimulate the muscle to relax and hold more urine. No weakening. No double hit. A 2022 study in European Urology found only a 4% retention rate with mirabegron in men with mild BPH-compared to 18% with anticholinergics. The FDA approved vibegron in 2020 specifically for patients who can’t tolerate anticholinergics.
Who Might Still Get Anticholinergics? (And How)
Not every man with BPH is automatically off-limits. Some urologists, like Dr. Kenneth Kobashi, argue that in carefully selected cases-men with mild BPH, strong urine flow, and no history of retention-low-dose solifenacin can be tried under strict monitoring.
But “carefully selected” means more than just a quick chat. Before even considering an anticholinergic, your doctor should check:
- Digital rectal exam to measure prostate size
- Uroflowmetry to see how fast you urinate (a peak flow under 10 mL/sec means high risk)
- Post-void residual to see how much urine is left after you go (over 150 mL is a red flag)
If any of these are abnormal, anticholinergics are a no-go. Even if they’re normal, start with the lowest dose and monitor closely. Monthly uroflow tests are not optional-they’re essential.
Yet, a 2019 report from the American Geriatrics Society found that 40% of nursing home residents with BPH or urinary retention are still being prescribed anticholinergics. This isn’t just outdated-it’s dangerous.
What to Do If You’re Already on an Anticholinergic
If you’re taking one of these drugs and have BPH, don’t stop cold turkey. Talk to your doctor. But do ask these questions:
- Have I had my urine flow and post-void residual tested since I started this?
- Is my prostate size known? Is it over 30 grams?
- What’s my AUA symptom score? Is it above 20?
- Have we considered tamsulosin or vibegron instead?
If you suddenly can’t urinate at all-no drip, no stream, just pressure-that’s an emergency. Go to the ER. Don’t wait. Acute retention needs immediate catheterization. Studies show waiting makes recovery harder. The bladder doesn’t recover well after being overstretched.
After catheterization, your doctor should start you on an alpha-blocker like tamsulosin. That boosts your chance of passing a voiding trial by 40%. Skipping this step? You’re likely to be back in the hospital within a week.
The Bottom Line
Anticholinergics aren’t evil drugs. They help people without prostate issues. But for men with BPH, they’re a ticking time bomb. The benefits are small. The risks are big. And the alternatives are better, safer, and proven.
Doctors still prescribe them because they’re familiar. Patients take them because they’re told, “It’s just for urgency.” But urgency isn’t worth a catheter. It’s not worth surgery. It’s not worth losing your dignity in the ER.
Ask for a uroflow test. Ask about vibegron. Ask if your prostate has been measured. If your doctor pushes back, get a second opinion. Your bladder doesn’t need another enemy.
What’s Next for Treatment?
Research is moving fast. The National Institute of Diabetes and Digestive and Kidney Diseases is funding a study through 2025 to predict who can safely use anticholinergics using prostate MRI scans and genetic markers. The goal? Personalized medicine-so no one gets hit with a drug that could shut down their bladder.
For now, the message is clear: If you have an enlarged prostate, anticholinergics are not your friend. There are better, safer ways to manage urgency. Use them.




Jean Claude de La Ronde
December 11, 2025 AT 13:37so like... if your bladder is a stubborn mule and the doc gives you a whip made of lead? yeah. that’s not therapy, that’s a prank. why do we still let doctors prescribe drugs that turn your pee hole into a locked vault? 🤡
Jim Irish
December 12, 2025 AT 10:19This is an important discussion. Many elderly men are unaware of the risks associated with anticholinergics. Safe alternatives exist and should be prioritized. Medical education must improve in this area.
john damon
December 14, 2025 AT 08:38bro i was on oxybutynin for 3 months 😭 my bladder just said ‘nope’ and shut down. ER at 3am. catheter. felt like a robot. now i take tamsulosin and i’m basically a new man 🙌
Katherine Liu-Bevan
December 14, 2025 AT 08:44Studies consistently show that men with BPH and a post-void residual over 150 mL should never be prescribed anticholinergics. Yet, 40% of nursing home residents still are. This is a systemic failure in geriatric prescribing practices. Uroflowmetry and digital rectal exams are simple, low-cost tools that are routinely ignored. Patients deserve better. Always ask for baseline urodynamic testing before starting any anticholinergic. It’s not just prudent-it’s standard of care.
Mia Kingsley
December 14, 2025 AT 12:36ok but like... who even decided that blocking acetylcholine was a good idea for a prostate problem? this is like giving someone a broken leg a wheelchair and calling it a cure. also vibegron is just fancy marketing for ‘we gave up on fixing the plumbing’
Kristi Pope
December 15, 2025 AT 00:06thank you for writing this. i’ve been scared to say anything because everyone just says ‘take the pill’ but my bladder’s been screaming for months. i asked my doc about mirabegron and they looked at me like i was speaking alien. i’m going back with this article printed out. you’re not alone.
Courtney Blake
December 15, 2025 AT 06:58another anti-pharma rant. these drugs are safe if used correctly. you’re just scared of big pharma because you watch too many YouTube videos. also, tamsulosin causes dizziness and fainting-did you forget that? at least anticholinergics don’t make you fall down stairs.
Lisa Stringfellow
December 16, 2025 AT 22:16why are you even writing this? nobody cares. everyone knows these drugs are dangerous. but doctors don’t care. patients don’t care. insurance won’t pay for the good stuff. it’s all just noise. just take your pills and shut up.
Sylvia Frenzel
December 18, 2025 AT 09:58the fact that we’re still having this conversation in 2025 is embarrassing. we have MRI scans, genetic markers, AI algorithms-but we still let doctors prescribe a drug that causes urinary retention like it’s a side effect you just ‘tough out’? this isn’t medicine. this is negligence dressed in a white coat.
Paul Dixon
December 19, 2025 AT 23:05man i had no idea. my dad’s on solifenacin and he’s been ‘holding it’ for weeks. i thought he was just being stoic. i’m printing this out and handing it to him tomorrow. thanks for the heads up.
matthew dendle
December 20, 2025 AT 18:58you guys are overthinking this. just get the catheter out and call it a day. anticholinergics are fine. if your bladder cant handle it then maybe you should’ve eaten less soup in your 50s 😴