
When you take an antiviral medication-whether for HIV, hepatitis C, or another viral infection-you’re not just dealing with one drug. You’re dealing with a system. A complex, invisible network inside your body that decides how much of the drug gets in, how long it stays, and how it interacts with everything else you’re taking. Two key players in this system are CYP3A4 and P-glycoprotein. Ignore them, and you risk serious side effects. Understand them, and you can take your meds safely-even with other prescriptions, supplements, or even food.
Why CYP3A4 and P-glycoprotein Matter
CYP3A4 is the most common enzyme in your liver and gut that breaks down drugs. About half of all medications you take pass through it. P-glycoprotein (P-gp) is a pump that kicks drugs out of cells, especially in the gut, brain, and kidneys. Together, they control how much of a drug actually reaches your bloodstream and stays there long enough to work. For antivirals, this isn’t just background science. It’s life-or-death. Many antivirals-like ritonavir, darunavir, glecaprevir, and sofosbuvir-are either broken down by CYP3A4 or pushed out by P-gp. If something else blocks or speeds up these systems, your drug levels can crash… or spike dangerously high.How Boosters Like Ritonavir Work
Ritonavir was originally designed as an HIV drug. But doctors noticed something strange: when they gave it in low doses-just 100 mg a day-it didn’t kill the virus well, but it made other HIV drugs work way better. Why? Because ritonavir is a powerful CYP3A4 inhibitor. It shuts down the enzyme, so other drugs aren’t broken down as fast. That means more of them stay in your blood. It also blocks P-glycoprotein. That means more of the drug gets absorbed from your gut. The result? A single pill of darunavir/ritonavir can be as effective as taking three or four separate pills. But here’s the catch: ritonavir doesn’t just inhibit CYP3A4. It also induces another enzyme, CYP1A2. That means it can make some drugs work less well-even while making others stronger. This dual effect is why some patients on ritonavir see their anxiety meds drop in effectiveness, while their blood thinners become dangerously potent.Real-World Risks: When Interactions Turn Dangerous
A 68-year-old man on apixaban for atrial fibrillation started taking darunavir/cobicistat for HIV. Within weeks, he had severe internal bleeding. His anti-Xa levels-normally between 50 and 250 ng/mL-shot up to 384. That’s not a typo. That’s life-threatening. This isn’t rare. A 2021 study in The Lancet Infectious Diseases found that 17.3% of adverse drug events in HIV and hepatitis C patients were caused by unmanaged drug interactions. Many of these involved CYP3A4 or P-gp. Some combinations are outright dangerous:- Simvastatin + paritaprevir/ritonavir/ombitasvir/dasabuvir → 1,760% increase in simvastatin levels → risk of muscle breakdown
- Grazoprevir + cyclosporine → 17.3-fold increase in grazoprevir levels → liver damage
- St. John’s wort + ritonavir → 57% drop in ritonavir levels → risk of HIV resistance
Not All Antivirals Are Created Equal
Some antiviral regimens are interaction nightmares. Others are much cleaner. Take the older hepatitis C combo: paritaprevir/ritonavir/ombitasvir/dasabuvir. It required dose changes or avoidance of 42% of common medications. That’s nearly half of everything you might be on. Now compare it to glecaprevir/pibrentasvir. It only needs adjustments for 17% of common drugs. Why? Because it doesn’t rely on ritonavir. It’s built to be less disruptive. For HIV, cobicistat is now often used instead of ritonavir as a booster. It’s just as strong at inhibiting CYP3A4-but it doesn’t induce CYP1A2. That means fewer conflicting effects. But it’s not perfect: cobicistat can raise creatinine levels, which can trick doctors into thinking kidney function is worse than it is. Sofosbuvir, a hepatitis C drug, barely touches CYP3A4. But it’s a P-gp substrate. So if you’re on a strong P-gp blocker like verapamil or quinidine, your sofosbuvir levels can rise. Not usually dangerous-but something you still need to check.What You Should Do Before Starting Any Antiviral
You can’t guess your way out of this. You need a system.- Make a full list of every medication, supplement, and herbal product you take-even over-the-counter painkillers, antacids, or sleep aids.
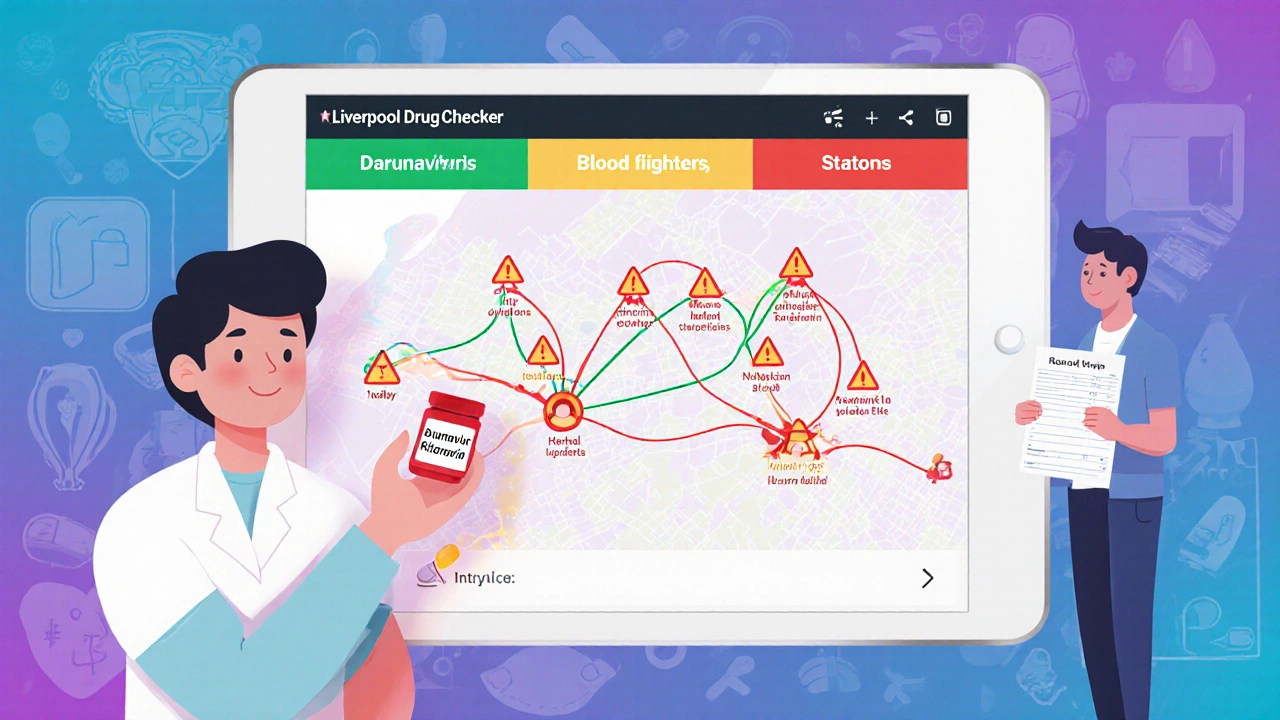
- Use the University of Liverpool HIV Drug Interactions Checker-it’s free, web-based, and used by clinics worldwide. It tells you if your combo is green (safe), yellow (monitor), or red (avoid).
- Ask your pharmacist to run a full interaction screen. Most pharmacies can do this in minutes.
- Don’t assume natural = safe. St. John’s wort, garlic supplements, and even some green tea extracts can interfere.
- Time matters. If you’re starting a blood thinner or statin, wait at least a month after beginning your antiviral. This lets your body stabilize before adding another drug.

What Clinicians Are Doing Differently Now
In 2022, a study in HIV Medicine tracked 347 patients using the Liverpool app. Before the app, 18.7% had interaction-related side effects. After six months of routine screening, that dropped to 5.2%. That’s a 72% reduction. Hospitals in Europe now have automated alerts in their electronic records. If you’re prescribed darunavir and warfarin, the system flags it. In the U.S., adoption is slower-but growing. Mayo Clinic saw a 31% drop in severe interactions after adding DDI alerts to their Epic system. But the biggest shift? Doctors no longer just check for CYP3A4. They’re now trained to look at transporters too-OATP1B1, BCRP, OCT2. A 2022 study found that 22% of serious adverse events came from these overlooked pathways.What’s Coming Next
New antivirals like lenacapavir are being designed to avoid CYP and transporter interactions entirely. That’s a game-changer. But we’re not there yet. Genetic testing is also becoming part of the picture. If you have the CYP3A5*3/*3 genotype (common in 85% of white people), your body processes some drugs much slower when combined with ritonavir. That can mean double the drug exposure. Testing for this isn’t routine yet-but it’s coming. And with 39 million people on antivirals by 2025, according to UNAIDS, the problem isn’t shrinking. It’s growing. More people. More medications. More comorbidities. The average person with HIV now has 4.7 other chronic conditions. Managing interactions isn’t a side note anymore. It’s the core of treatment.Bottom Line: Don’t Guess. Check.
Antiviral medications are powerful. But they’re not magic. They play by rules-and those rules involve enzymes and pumps you can’t see. One wrong combo can send you to the hospital. One simple check can keep you safe. If you’re on an antiviral, don’t wait for your doctor to ask. Bring your full list of meds to every appointment. Use the Liverpool app. Talk to your pharmacist. And if something feels off-like unusual bruising, muscle pain, or extreme drowsiness-speak up. Your life might depend on it.Can I take grapefruit juice with my antiviral medication?
No, it’s not safe. Grapefruit juice contains bergamottin, which blocks CYP3A4 in your gut. This can raise levels of antivirals like ritonavir, darunavir, and others by up to 23%. That may lead to toxicity, including liver damage or severe side effects. Even small amounts-like half a glass-can have an effect. Stick to water or non-grapefruit juices.
Does St. John’s wort interfere with antivirals?
Yes, dangerously. St. John’s wort activates enzymes that break down antivirals, especially ritonavir. Studies show it can drop ritonavir levels by 57%, which increases the risk of HIV or hepatitis C becoming resistant to treatment. It can also reduce the effectiveness of other antivirals like sofosbuvir. Never take it with antivirals without talking to your doctor first.
Are newer antivirals safer than older ones?
Generally, yes. Older regimens like paritaprevir/ritonavir/ombitasvir/dasabuvir required dose changes for 42% of common medications. Newer options like glecaprevir/pibrentasvir and lenacapavir have far fewer interactions. Some, like lenacapavir, are designed to avoid CYP3A4 and P-gp entirely. But even newer drugs aren’t risk-free-always check interactions before starting any new medication.
Why does my doctor keep asking about my other medications?
Because antivirals interact with almost everything. Blood thinners, statins, antidepressants, even common painkillers like ibuprofen or omeprazole can change how your antiviral works. A drug that’s safe alone can become dangerous when combined. Your doctor isn’t being overly cautious-they’re preventing a potentially life-threatening reaction. A 2021 study showed 17.3% of adverse events in HIV/hepatitis patients were due to uncaught interactions.
Can I use a free app to check for drug interactions?
Yes, and you should. The University of Liverpool HIV Drug Interactions Checker is free, trusted by clinics worldwide, and updated monthly. It gives you color-coded results: green (safe), yellow (monitor), red (avoid). It’s used by over 1.2 million people and has 98.7% accuracy compared to expert panels. Download it, enter your meds, and share the results with your doctor.
What should I do if I start a new medication while on an antiviral?
Stop. Don’t start it until you’ve checked. Even if it’s something as simple as a new allergy pill or sleep aid, it could interact. Use the Liverpool app or call your pharmacist. Wait 24 hours after checking before taking the new drug. If you’ve already started it, monitor for side effects-like unusual bleeding, muscle pain, dizziness, or nausea-and contact your provider immediately.
Is it safe to take herbal supplements with antivirals?
Most are not. Herbal supplements are not regulated like drugs, and many affect CYP3A4 or P-gp. Garlic, milk thistle, turmeric, and ginseng can all interfere. Some reduce antiviral levels (risking resistance), others raise them (risking toxicity). Always tell your doctor about every supplement you take-even if you think it’s harmless.
Why do some antivirals need a booster like ritonavir or cobicistat?
Boosters like ritonavir and cobicistat are used to slow down how quickly your body breaks down the main antiviral drug. This allows lower doses of the main drug to work just as well, reduces pill burden, and improves effectiveness. But they come with trade-offs: they increase the risk of drug interactions and side effects. Newer antivirals are being developed without boosters to avoid these problems.




Kane Ren
November 21, 2025 AT 13:39Just took my new hepatitis C meds last week and was about to grab my usual grapefruit smoothie-glad I read this first. Seriously, this post saved me from a hospital trip. Thanks for laying it out so clearly.
Also, the Liverpool app? Downloaded it. Already flagged two of my supplements. Lifesaver.
Charmaine Barcelon
November 23, 2025 AT 08:48You people are so naive!! You think grapefruit juice is ‘harmless’?!! It’s not!! It’s a chemical bomb in a glass!! And don’t even get me started on St. John’s wort-IT’S NOT A ‘SUPPLEMENT,’ IT’S A DRUG!! Your ‘natural’ nonsense is killing people!!
And why are you all still taking ibuprofen?! It’s a disaster waiting to happen with antivirals!! STOP IT!!
Karla Morales
November 24, 2025 AT 06:27📊 Data point: 17.3% of adverse events in HIV/HCV patients stem from unmanaged CYP3A4/P-gp interactions (Lancet, 2021).
📉 The Liverpool app reduced interaction-related side effects by 72% in a 347-patient cohort (HIV Medicine, 2022).
⚠️ Ritonavir + simvastatin = 1,760% increase in simvastatin AUC. That’s not a typo. That’s rhabdomyolysis waiting to happen.
💡 Pro tip: Cobicistat doesn’t induce CYP1A2-unlike ritonavir. That’s why it’s becoming the new standard. But it still elevates creatinine-so don’t mistake it for renal decline.
🧬 CYP3A5*3/*3 genotype carriers? You’re looking at 2x drug exposure. Genetic testing is no longer optional-it’s clinical best practice.
🩺 Bottom line: If you’re on antivirals, your pharmacy should be running a full DDI screen monthly. Not quarterly. Monthly.
✅ TL;DR: Don’t guess. Check. Document. Repeat.
Javier Rain
November 25, 2025 AT 21:32This is the kind of post that makes me believe in the internet again. Seriously. I’ve been on HIV meds for 8 years and never knew grapefruit juice could mess with my regimen. I thought it was just ‘good for you.’
Just called my pharmacist-she ran my whole list through the Liverpool app and found a red flag with my OTC sleep aid. We swapped it out in 10 minutes.
Don’t wait until you’re bleeding internally. Do the check. Now. Your future self will high-five you.
Also-shoutout to the docs who are finally looking at transporters like OATP1B1. We’ve been ignoring those for too long. Progress!
Laurie Sala
November 27, 2025 AT 07:29I just cried reading this… I had to stop taking my turmeric capsules last year because I started getting muscle pain… I didn’t know why… I thought it was just aging… I wish I’d known this sooner…
My mom died from internal bleeding after starting a new antiviral… she never told her doctor about her fish oil… I’m so angry… and so sad…
Please… please… if you’re reading this… check your meds… I beg you…
Lisa Detanna
November 27, 2025 AT 20:18As someone who’s lived in three countries and taken antivirals in each, I can say this: the U.S. is ahead on DDI awareness, but Europe has better integration into EHRs. In Germany, my pharmacist flagged an interaction before my doctor even saw the script.
And in the Philippines, I saw people taking garlic supplements with HIV meds and thinking it ‘boosts immunity.’ No. It doesn’t. It breaks your treatment.
This isn’t just a medical issue-it’s a cultural one. We need better public education, not just apps. Talk to your community. Share this. It matters.
John Mackaill
November 28, 2025 AT 12:05One thing I wish more people knew: it’s not just about the drugs you’re taking-it’s about the timing. Starting a statin too soon after an antiviral? Big mistake. Give it a month. Let your body stabilize.
Also, don’t assume your doctor knows everything. I’ve had mine miss interactions twice before I pulled up the Liverpool app and showed them the red flag. You have to be your own advocate.
Adrian Rios
November 29, 2025 AT 10:05Let me tell you what really freaked me out-when I found out that my daily omeprazole, which I thought was just ‘safe for stomach issues,’ was reducing my sofosbuvir absorption by 40%. I’d been on it for six months. No one told me.
And then I learned that even green tea extract can interfere with P-gp. I used to drink three cups a day. Now? Zero. Just water. I’ve been doing this for a year. No side effects. No surprises.
And honestly? I used to think ‘natural’ meant ‘safe.’ Now I know better. I’m not just taking meds-I’m managing a chemical ecosystem. It’s not magic. It’s science. And science doesn’t care how ‘healthy’ you think your diet is.
So I made a spreadsheet. Every pill. Every supplement. Every tea. Every juice. I update it every Sunday. I print it. I bring it to every appointment. I show it to the pharmacist. I don’t trust memory. I trust paper.
And guess what? My last lab results were the best they’ve ever been. I’m not just surviving. I’m thriving. Because I stopped guessing. And started checking.
If you’re on antivirals? Do the same. You’re worth the effort.
Casper van Hoof
November 30, 2025 AT 20:48One might argue that the CYP3A4/P-gp paradigm is a reductionist framework-yet it remains the most empirically validated model for predicting pharmacokinetic interactions in clinical practice.
While newer agents like lenacapavir represent a paradigm shift toward transporter-agnostic design, the historical dominance of ritonavir as a pharmacokinetic enhancer reflects not merely therapeutic necessity, but also the inertia of pharmaceutical development pipelines rooted in 20th-century enzymology.
Thus, the imperative to screen for interactions is not merely clinical-it is epistemological: our understanding of drug behavior is still tethered to a limited set of molecular pathways, even as polypharmacy becomes the norm in aging populations.
Until pharmacogenomics becomes standard, the Liverpool tool remains not merely a utility, but a moral artifact-a digital conscience in an age of therapeutic complexity.