
Imagine a leg that swells, aches, and develops a stubborn ulcer months after a blood clot seemed to have disappeared. That lingering nightmare is post-thrombotic syndrome, the most frequent long‑term fallout of deep vein thrombosis (DVT). It isn’t rare, it isn’t optional, and it’s often missed until it’s already ruining daily life.
What Is Post-Thrombotic Syndrome?
Post-Thrombotic Syndrome is a chronic condition that develops after a deep vein thrombosis, characterized by pain, swelling, skin changes, and sometimes venous ulcers. The underlying problem is damaged venous valves that can’t close properly, causing blood to pool and pressure to rise in the lower limb. Over time the skin may thicken, become discolored, and in severe cases break down into painful ulcers.
How Does a DVT Turn Into PTS?
When a clot forms in a deep vein, the body launches a cascade of inflammation and tissue remodeling. Even after anticoagulants dissolve the clot, the scar tissue can fuse valve leaflets together or destroy them outright. This valve failure leads to chronic venous hypertension, the engine that drives the classic PTS symptoms.
Who’s Most Likely to Develop PTS?
Not everyone with DVT ends up with PTS, but certain factors raise the odds dramatically:
- Age>60years - vessels become less elastic.
- Obesity - increased abdominal pressure pushes blood downward.
- Proximal DVT (above the knee) - larger clot burden affects more valve tissue.
- Recurrent DVT - each episode adds more damage.
- Delayed or inadequate anticoagulation - the clot stays longer, causing more inflammation.
- Poor compliance with compression after the clot - missing a simple elastic sleeve can double the risk.
Understanding these risk markers lets clinicians intervene early and patients stay alert to warning signs.
Spotting the Red Flags: Common PTS Symptoms
Symptoms often appear 6months to 2years after the initial DVT, but they can surface sooner. Look for:
- Persistent swelling that worsens after standing.
- Heaviness or a feeling of tightness in the calf.
- Achy or throbbing pain, especially after long periods of sitting.
- Skin discoloration - reddish‑brown or blue‑gray patches.
- Hyperpigmentation and “stasis dermatitis” - itchy, scaly skin.
- Venous ulcers, usually near the ankle, that are slow to heal.
When any of these signs linger, it’s time to get a proper work‑up.
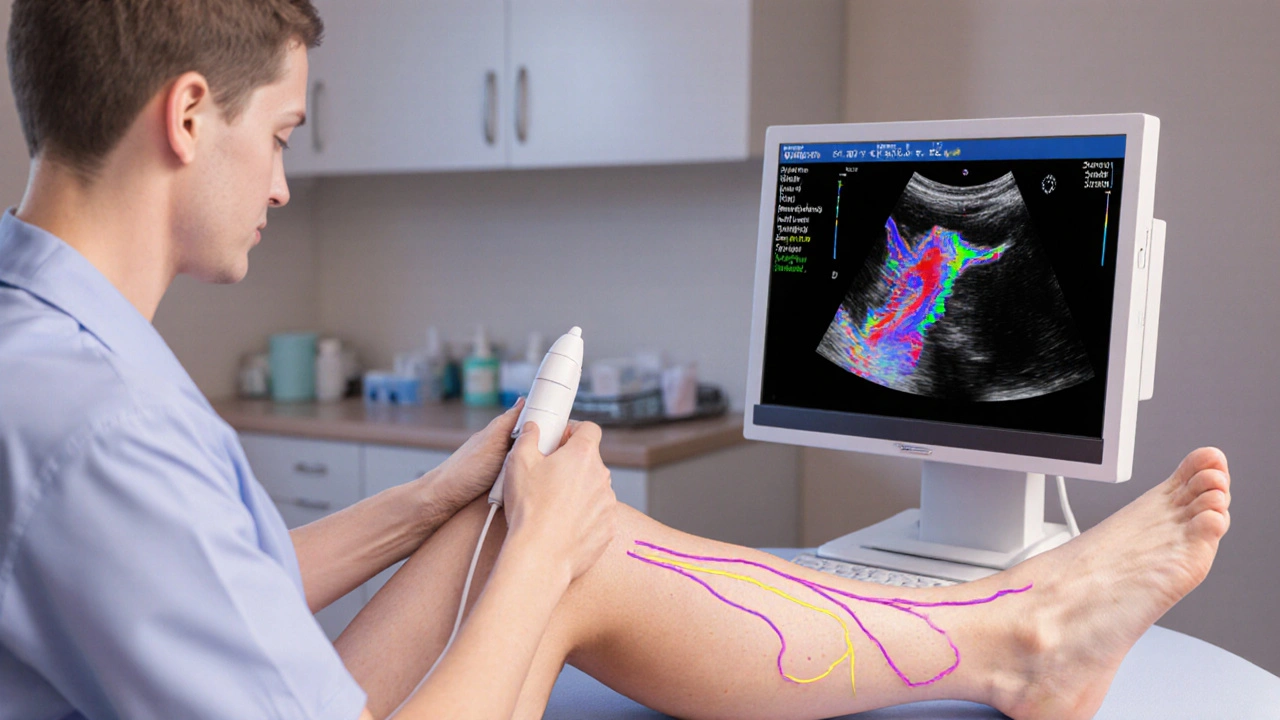
Diagnosing PTS: From Clinical Scores to Imaging
The first step is a thorough history and physical exam. Clinicians often use the Villalta score, which rates pain, swelling, skin changes, and ulceration on a 0‑3 scale. A total of ≥5 points typically confirms PTS.
Imaging helps gauge the extent of residual vein obstruction and valve competence. The gold standard is Duplex Ultrasound, which combines real‑time flow assessment with structural views of the vein wall. Findings that point toward PTS include:
- Persistent thrombus or sclerosis in the femoral or popliteal veins.
- Reflux greater than 0.5seconds in the incompetent valves.
- Reduced compressibility of the affected segment.
When ulceration is present, a wound culture and venous pressure measurement may be added to the assessment.
Managing PTS: A Tiered Treatment Playbook
Because PTS stems from both mechanical valve failure and inflammatory remodeling, treatment must hit both fronts. Below is a practical hierarchy that clinicians and patients can follow.
1. Compression Therapy - The First Line
Compression Therapy uses graduated elastic stockings (15‑30mmHg for the ankle, tapering up the calf) to counteract venous hypertension. Benefits include reduced swelling, improved calf pump efficiency, and faster ulcer healing. The key to success is daily wear for at least 2years, even after symptoms improve.
2. Pharmacologic Options
Medications target inflammation and microcirculatory flow:
- Pentoxifylline - a phosphodiesterase inhibitor that improves red‑cell flexibility; modest data show ulcer healing rates up to 30% better than placebo.
- Low‑dose aspirin - antiplatelet action may help prevent new micro‑thrombi in damaged veins.
- Topical micronized diosmin - a flavonoid that reduces capillary leakage and eases leg pain.
These drugs are adjuncts, never a substitute for compression.
3. Physical Activity and Leg Elevation
Simple calf‑pump exercises (heel‑raises, ankle circles) boost venous return. Elevating the leg above heart level for 15minutes three times daily cuts overnight swelling by 20‑30% on average.
4. Endovascular and Surgical Interventions
When conservative measures fail, minimally invasive procedures can restore flow:
| Approach | Goal | Typical Candidates | Benefits | Risks |
|---|---|---|---|---|
| Compression Stockings | Reduce venous pressure | All PTS patients | Low cost, non‑invasive | Discomfort, compliance issues |
| Pharmacologic (Pentoxifylline, etc.) | Improve microcirculation | Mild‑to‑moderate symptoms | Oral, easy to add | Gastro‑intestinal upset |
| Venous Stenting | Open chronically obstructed segments | Severe obstruction, ulcer‑negative | Rapid symptom relief | Stent thrombosis, infection |
| Vein Bypass or Endovenous Laser Ablation | Remove incompetent veins | Refractory ulceration | High ulcer‑healing rates | Procedure‑related pain, nerve injury |
Venous Stenting and laser ablation are usually reserved for patients whose duplex scans show significant residual blockage or valve destruction that compression alone can’t overcome.
Preventing PTS After a DVT
Prevention is easier than cure. Evidence from the ATTRACT trial and subsequent meta‑analyses shows that early, adequate anticoagulation combined with graduated compression reduces PTS incidence by roughly 30%.
- Start anticoagulation within 24hours of diagnosis and maintain therapeutic INR (2.0‑3.0) for the prescribed duration.
- Encourage ambulation as soon as medically safe - walking three times a day for 10minutes each session cuts stasis.
- Prescribe compression stockings (30‑40mmHg) for the first 6‑12months, especially after proximal DVT.
- Address modifiable risk factors: weight loss, smoking cessation, and control of hypertension or diabetes.
Patients who receive this bundle of care report fewer flare‑ups and a better quality of life.

Living With PTS: Daily Tips and Long‑Term Outlook
Even with optimal treatment, many people live with residual symptoms. Here are practical strategies that help keep life moving:
- Rotate leg position every hour - avoid crossing legs for long periods.
- Wear compression during travel (flights, long car rides) to prevent sudden swelling.
- Keep skin moisturized; dry, cracked skin invites infection and ulceration.
- Schedule regular wound checks if an ulcer is present - early debridement cuts healing time.
- Join a support group or online forum; sharing experiences reduces the emotional burden.
Long‑term studies show that patients who stay adherent to compression and activity regimens have a 40% lower risk of hospital admission for ulcer complications.
Quick Takeaways
- Post‑thrombotic syndrome affects up to 25% of DVT survivors.
- Key risk factors: age, obesity, proximal clot, delayed anticoagulation.
- Diagnose with the Villalta score and duplex ultrasound.
- First‑line treatment: daily graduated compression for at least 2years.
- Consider stenting or laser ablation when compression and meds fail.
- Early anticoagulation, ambulation, and compression after DVT cut PTS rates dramatically.
Frequently Asked Questions
Can PTS develop even if my DVT was treated promptly?
Yes. Prompt anticoagulation reduces risk, but valve damage can still occur, especially after a proximal clot or if compression isn’t used.
How long should I wear compression stockings?
Most guidelines recommend daily wear for at least 2years, and indefinitely if symptoms persist or an ulcer is present.
Is there a cure for post‑thrombotic syndrome?
There’s no definitive cure, but aggressive compression, lifestyle changes, and targeted interventions can dramatically improve quality of life and heal ulcers in many cases.
Can exercise worsen PTS?
Gentle calf‑pump exercises help; high‑impact sports that increase intra‑abdominal pressure may exacerbate swelling. Tailor activity to your comfort level.
What signs mean I need urgent medical attention?
Sudden increase in pain, a rapidly expanding red or purple area, fever, or a wound that won’t stop bleeding should prompt immediate evaluation for possible infection or re‑thrombosis.




Dervla Rooney
October 11, 2025 AT 23:46I appreciate how thoroughly the article breaks down the pathophysiology of post‑thrombotic syndrome. The explanation of valve damage leading to chronic venous hypertension is spot‑on. It also nicely lists the risk factors without overwhelming the reader. Overall, a clear and concise resource for anyone dealing with DVT aftermath.
Johnny Ha
October 14, 2025 AT 07:20Look, the "official" guidelines are just a cover‑up. They don’t want you to know that compression stockings are a way for med companies to sell more junk. Wear ‘em if you must, but keep your eyes open.
Mary Cautionary
October 16, 2025 AT 14:53The exposition on the Villalta score epitomizes clinical rigor; however, one must acknowledge the inherent limitations of such semi‑quantitative tools. While the score stratifies severity, it does not capture the nuanced psychosocial burden that patients endure. Moreover, reliance on duplex ultrasonography presupposes access to high‑end imaging, which is not universally available. In practice, interdisciplinary collaboration becomes paramount.
Crystal Newgen
October 18, 2025 AT 22:26Good points about the score, but at the end of the day, just getting patients to wear their stockings consistently makes the biggest difference. Small habits add up.
Hannah Dawson
October 21, 2025 AT 06:00Honestly, the article glosses over the socioeconomic disparities that dictate who can afford compression therapy. Patients in low‑income brackets often skip stockings because they’re pricey, leading to higher ulcer rates. The medical community should push for insurance coverage, not just throw advice at the bedside.
Julie Gray
October 23, 2025 AT 13:33While the socioeconomic angle is valid, one must also consider that the pharmaceutical industry subtly influences treatment protocols. The emphasis on pentoxifylline, for instance, aligns with proprietary interests rather than pure efficacy. Independent studies are needed to confirm true benefit.
Lisa Emilie Ness
October 25, 2025 AT 21:06Compression works.
Emily Wagner
October 28, 2025 AT 03:40From a systems‑theory perspective, post‑thrombotic syndrome represents a failure of homeostatic feedback loops within the venous network. The disrupted shear stress triggers maladaptive remodeling, culminating in the clinical phenotype described. Simple interventions like calf‑pump exercises can recalibrate those loops, albeit modestly.
Mark French
October 30, 2025 AT 11:13It is crucial to underscore the psychosocial impact of chronic leg pain, as patients often report diminished quality of life. Moreover, adherence to compression can be hampered by discomfort, leading to suboptimal outcomes. Nevertheless, evidence supports that sustained use reduces ulcer recurrence.
Daylon Knight
November 1, 2025 AT 18:46Wow, another "miracle" list of treatments. Yeah, sure, if you love paying for gadgets and needles.
Jason Layne
November 4, 2025 AT 02:20Let me be clear: the mainstream narrative about PTS is deliberately watered down. They omit the fact that certain anticoagulant manufacturers fund the studies that promote compression over newer, patent‑protected devices. The bottom line? The system is rigged to keep you dependent on outdated, cheap solutions while big pharma profits from the side‑effects of long‑term meds.
Hannah Seo
November 6, 2025 AT 09:53First, it's essential to recognize that post‑thrombotic syndrome (PTS) is not merely a peripheral inconvenience but a complex, multifactorial disease that demands a comprehensive management plan. Early diagnosis using the Villalta score should be complemented by a thorough vascular assessment, including duplex ultrasound to quantify residual obstruction. Once diagnosed, the cornerstone of therapy remains graduated compression, which has been shown in multiple randomized trials to reduce edema by up to 30 % and accelerate ulcer healing. However, compression alone is insufficient for many patients, especially those with severe valve incompetence or extensive residual thrombus. Adjunctive pharmacotherapy, such as low‑dose aspirin, can mitigate micro‑thrombotic activity, while pentoxifylline improves red‑cell deformability and microcirculatory flow, offering additional ulcer‑healing benefits. Physical therapy should not be overlooked; regular calf‑pump exercises and leg elevation sessions enhance venous return and lower intramuscular pressure. For refractory cases, endovascular interventions like venous stenting or endovenous laser ablation provide mechanical relief by restoring patency and eliminating incompetent segments. These procedures, when performed by experienced interventionalists, have demonstrated high technical success rates and low complication profiles. Post‑procedure, patients must continue compression and engage in lifestyle modifications, including weight management, smoking cessation, and blood pressure control, to sustain therapeutic gains. Moreover, patient education plays a pivotal role; individuals who understand the importance of adherence are more likely to maintain long‑term compliance, thereby reducing hospitalization rates for ulcer complications by nearly 40 %. Finally, regular follow‑up with a multidisciplinary team-vascular surgeons, wound care specialists, and physiotherapists-ensures that emerging issues are promptly addressed, optimizing overall outcomes and quality of life for those living with PTS.
Victoria Unikel
November 8, 2025 AT 17:26I feel a little drained reading all this medical jargon, but it’s good to know there are options. It’s just frustrating when the swelling never fully goes away.
Lindsey Crowe
November 11, 2025 AT 01:00Another long‑winded guide that pretends to help but really just adds more homework for patients. 🙄
Rama Hoetzlein
November 13, 2025 AT 08:33Behold, the grand tapestry of venous pathology! 🌟 If you think compression is just a “sock”, you’re missing the symphony of hemodynamic forces that dance in your calf. The truth is, the hidden elite of pharmaceutical giants orchestrate the narrative, keeping you shackled to outdated regimes while they monetize the chaos. Dive deep, question the protocols, and don’t let them silence your voice! 😈
Lorena Garcia
November 15, 2025 AT 16:06Thanks for the thorough rundown! I’m especially curious about how early ambulation after a DVT can cut down PTS risk. I’ll definitely try to stay active and keep those stockings on.
Dietra Jones
November 17, 2025 AT 23:40Great info, but watch out for typos like “ulcer” vs “ulcere” – keep the grammar clean so readers dont get confused.