
Rhabdomyolysis Risk Checker
Medication Safety Assessment
Your Risk Factors
Dangerous Drug Combinations Found
Imagine taking your daily statin for cholesterol, then adding an antibiotic for a sinus infection-only to wake up with dark urine, muscle pain so bad you can’t stand, and no idea why. This isn’t rare. It’s rhabdomyolysis, a dangerous condition where muscle tissue breaks down rapidly, flooding your bloodstream with toxins that can shut down your kidneys. And more often than not, it’s not the drug alone-it’s the combination that kills.
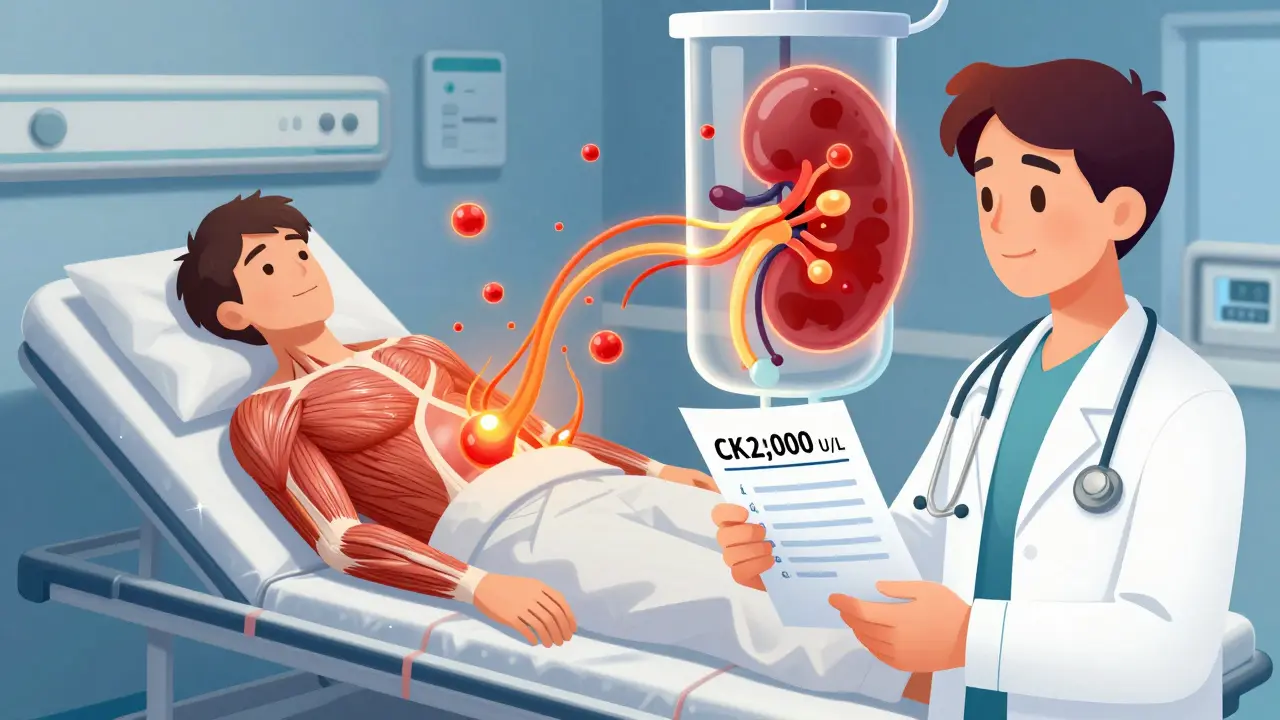
What Happens When Muscles Start Breaking Down
Rhabdomyolysis isn’t just sore muscles after a hard workout. It’s a medical emergency. When muscle cells rupture, they spill their contents-creatine kinase (CK), potassium, phosphate, and myoglobin-into your blood. Myoglobin is the real danger. Your kidneys filter it out, but in large amounts, it clogs the tiny tubes inside them. That’s how a simple drug mix can lead to acute kidney injury, dialysis, or even death.Most people think of rhabdomyolysis as something that happens after extreme exercise or trauma. But in hospitals, up to 10% of cases come from medications. And the most common culprits? Statins. These cholesterol-lowering drugs like atorvastatin and simvastatin are prescribed to millions. But when paired with other drugs, they turn toxic.
The Most Dangerous Drug Combinations
Not all drug interactions are created equal. Some are mild. Others are deadly. Here’s what actually puts you at risk:- Statin + Fibrates (especially gemfibrozil): This combo increases rhabdomyolysis risk by 15 to 20 times compared to statins alone. Gemfibrozil blocks how your body clears simvastatin, letting it build up to toxic levels.
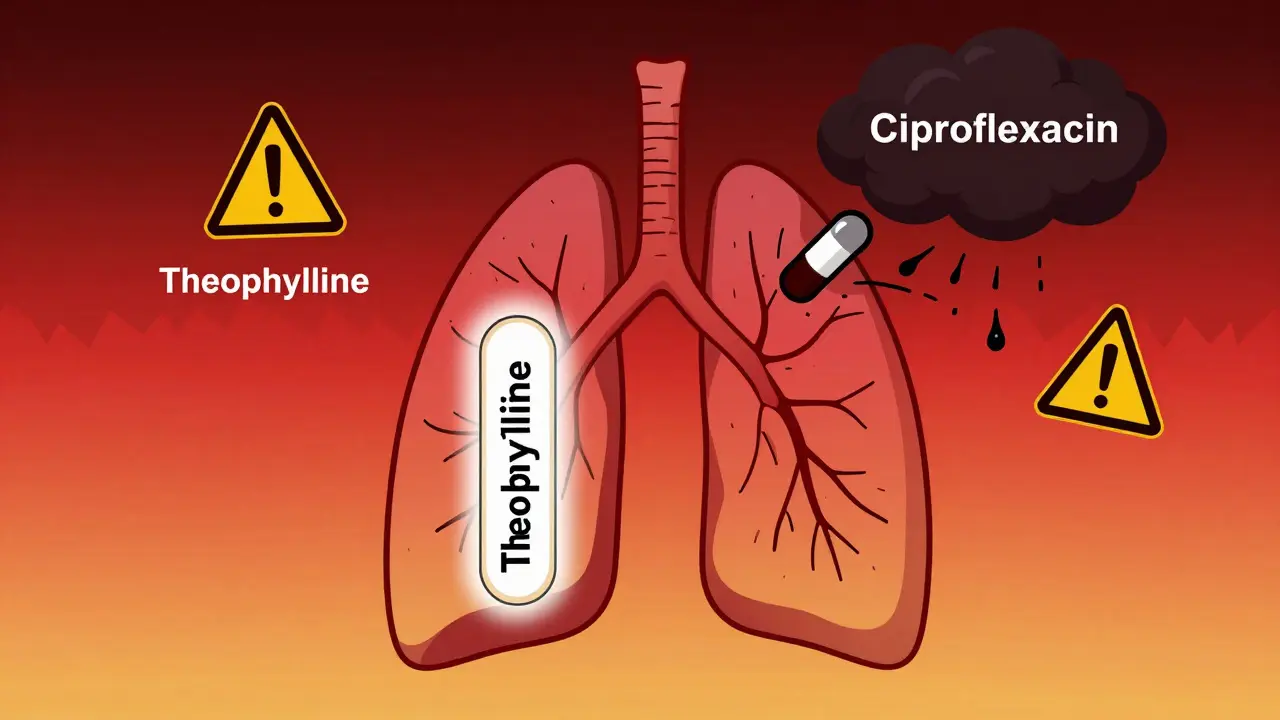
- Statin + Macrolide Antibiotics (like clarithromycin or erythromycin): These antibiotics block the CYP3A4 enzyme, which is how your liver breaks down statins. One study showed a 18.7-fold jump in risk with simvastatin and erythromycin.
- Colchicine + CYP3A4 Inhibitors (like clarithromycin or itraconazole): Used for gout, colchicine is already risky on its own. Add a strong inhibitor, and your risk of muscle breakdown jumps 14 times. The European Medicines Agency issued a formal warning in 2021 after reviewing over 1,200 cases.
- Statin + Antivirals (like erlotinib for lung cancer): This combo is rarely discussed but extremely dangerous. Case reports show CK levels over 20,000 U/L within 72 hours-enough to trigger kidney failure.
- Propofol in ICU patients: Though rare, this anesthetic can cause a lethal form of rhabdomyolysis by crippling mitochondria-the energy factories in your muscle cells. Mortality hits 68% when it happens.
And here’s the kicker: these interactions don’t always show up on standard drug interaction checkers. Many doctors don’t know the full list. Patients often aren’t warned.
Who’s at Highest Risk?
It’s not just about the drugs. Your body matters too.- Age 65+: Your liver and kidneys slow down. You’re 3.2 times more likely to develop rhabdomyolysis from the same dose.
- Women: Studies show women have a 1.7 times higher risk than men, even when taking the same meds.
- Chronic kidney disease: If your eGFR is below 60, your risk spikes 4.5 times. Your kidneys can’t handle the myoglobin load.
- On five or more medications: Polypharmacy is the silent killer. People taking 5+ drugs are 17 times more likely to experience this reaction, according to a 2022 JAMA study.
- Genetic risk: A common gene variant called SLCO1B1*5 makes it harder for your body to clear simvastatin. People with this variant have a 4.5-fold higher risk of muscle damage.
These aren’t rare outliers. They’re predictable patterns. And they’re avoidable-if you know what to look for.
Signs You Might Be in Trouble
The classic triad-muscle pain, weakness, and dark urine-only shows up in about half of cases. That’s why so many people miss it.More common early signs:
- Unexplained muscle soreness that doesn’t go away after a few days
- Urine that looks like cola, tea, or dark beer
- Feeling unusually tired, nauseous, or feverish without an infection
- Swelling or tightness in arms, legs, or back
- Sudden drop in urine output
One patient on Reddit wrote: “After adding clarithromycin to my colchicine for gout, my urine turned cola-colored within 48 hours. CK hit 28,500. I was in the ER before I even knew what was happening.”
Another: “My oncologist didn’t warn me about simvastatin and erlotinib. CK peaked at 42,000. I needed three days of dialysis.”
If you’re on any of the high-risk combos above and notice these symptoms, don’t wait. Go to the ER. Get a CK test.
How Doctors Diagnose and Treat It
There’s no single test that catches rhabdomyolysis early. But CK levels are the gold standard. Normal levels are under 200 U/L. Anything over 1,000 U/L is suspicious. Over 5,000 U/L means serious muscle breakdown. In severe cases, levels can hit 100,000 U/L or higher.Once diagnosed, treatment is urgent:
- Stop the offending drug immediately. No exceptions.
- Aggressive IV fluids. The goal? Flush out myoglobin before it damages your kidneys. Hospitals often give 3 liters of saline in the first 6 hours, then 1.5 liters per hour.
- Urine alkalinization. Adding sodium bicarbonate to IV fluids keeps urine pH above 6.5, which stops myoglobin from clumping in the kidneys.
- Monitor electrolytes. High potassium can cause cardiac arrest. Low calcium can trigger seizures. Both are common.
- Dialysis. If kidneys fail, you need it. About 50% of severe cases require it.
Some cases, like those caused by leflunomide (a rheumatoid arthritis drug), are so severe that plasma exchange is needed to remove the drug from the blood. It’s not just about hydration-it’s about removing the poison.
Why This Keeps Happening
You’d think doctors would know this. But they don’t always.A 2022 study in the American Journal of Emergency Medicine found that 92% of patients with statin-induced rhabdomyolysis had symptoms that were ignored or mislabeled as “just muscle soreness.” Many providers didn’t even check CK levels.
Pharmacies don’t always flag the interactions. Electronic health records often miss complex combinations. And patients? They’re told to take their pills and assume everything’s fine.
The FDA added black box warnings to statins in 2012. The EMA now requires specific contraindications on labels. But enforcement? Patchy. Prescriptions keep rising. Deaths keep happening.
What You Can Do Right Now
If you’re on any of these medications:- Check your list with your pharmacist. Ask: “Could any of these cause muscle breakdown?”
- Know your CK level. If you’ve had a recent blood test, ask for the number. If it’s above 1,000 and you’re on a high-risk combo, push for a review.
- Never start a new medication without asking about interactions. Even OTC drugs like ibuprofen or herbal supplements like red yeast rice (which acts like a statin) can add risk.
- Track your urine color. If it’s dark for more than a day, get it checked.
- If you’re over 65, have kidney issues, or take five or more meds-ask your doctor if you really need all of them.
There’s no magic pill to prevent this. But awareness saves lives. You don’t need to stop your statin. You just need to know what not to mix it with.
Long-Term Outlook
Recovery isn’t quick. Even if your kidneys bounce back, muscle damage lingers. Mayo Clinic’s 10-year follow-up found that 44% of survivors still had muscle weakness six months later. Full recovery took an average of 12 weeks for those without kidney failure-but nearly three months for those who needed dialysis.And the future? It’s getting riskier. As people live longer and take more drugs, rhabdomyolysis cases are projected to rise 8.2% per year through 2030. The NIH is funding research into real-time drug interaction alerts. But until then, the responsibility falls on you.
You’re not just a patient. You’re your own best advocate. Ask questions. Know your meds. Listen to your body. Dark urine isn’t dehydration. Muscle pain isn’t just aging. And sometimes, the thing that’s supposed to save you is quietly breaking you down.
Can you get rhabdomyolysis from just one statin, without any other drugs?
Yes, but it’s rare. About 40% of statin-related rhabdomyolysis cases happen without other drugs, usually in people over 65, with kidney problems, or those on high doses. The risk is still low-about 2.3 cases per 10,000 patient-years-but it’s real. That’s why doctors start with low doses and monitor CK levels in high-risk patients.
Are there any safe statin combinations?
Yes. Pravastatin and rosuvastatin are less likely to cause rhabdomyolysis because they’re not processed by the CYP3A4 enzyme. If you need a statin and are on other medications, ask your doctor about switching to one of these. They’re just as effective for lowering cholesterol but much safer when combined with antibiotics, antifungals, or other common drugs.
How long after starting a new drug does rhabdomyolysis usually appear?
Most cases occur within 30 days of starting or changing a dose. Statin-related cases typically show up around 28 days after starting the drug. But with strong interactions-like statin plus clarithromycin-symptoms can hit within 48 to 72 hours. Don’t wait. If you feel worse after starting a new pill, get checked.
Can supplements cause rhabdomyolysis?
Absolutely. Red yeast rice contains monacolin K, which is chemically identical to lovastatin. It’s sold as a “natural” cholesterol remedy but carries the same risks. Other supplements like creatine (in very high doses), niacin, and even green tea extract have been linked to cases. Always tell your doctor what you’re taking-even if you think it’s harmless.
Is rhabdomyolysis permanent?
Most people recover fully if treated early. But if kidney damage occurs, recovery takes longer-and some lose permanent kidney function. Muscle weakness can linger for months. In severe cases, nerve damage or chronic pain develops. The key is early detection. The sooner you stop the drug and start fluids, the better your chances.
Should I stop my statin if I’m on an antibiotic?
Don’t stop it yourself. Call your doctor or pharmacist immediately. If you’re on simvastatin or atorvastatin and prescribed clarithromycin, azithromycin, or an antifungal like itraconazole, ask if you can switch to pravastatin or rosuvastatin instead. If not, your doctor may pause the statin during the antibiotic course. Never guess-this interaction can be deadly.




Alexandra Enns
January 24, 2026 AT 07:23Wow. So let me get this straight - the FDA gives statins a black box warning, but doctors still prescribe them like candy? And pharmacists? They’re too busy scanning barcodes to read the damn labels. This isn’t medical care, it’s corporate roulette. I’m 62, on simvastatin and amoxicillin for a sinus thing - and nobody told me this could kill me. I’m canceling my next appointment until someone explains why this keeps happening. #BigPharmaIsKillingUs
Marie-Pier D.
January 25, 2026 AT 14:48Thank you for writing this. I’ve been terrified to even take my statin since my mom had rhabdo from a combo of gemfibrozil and atorvastatin. She was 71, had CK over 80,000, and spent 17 days in ICU. 😢 I finally asked my doctor to switch me to rosuvastatin - and she actually listened. 🙏 If you’re on meds, please, please ask about muscle risk. You’re not being difficult - you’re being smart.
Dolores Rider
January 26, 2026 AT 18:54Okay but have you heard about the 2018 CDC memo that got buried? The one that said statins were linked to 12,000+ deaths/year from rhabdo? They buried it because Medicare pays more for prescriptions than ER visits. The government knows. They just don’t care. 🤫💊
Jenna Allison
January 27, 2026 AT 08:39Just to clarify - CYP3A4 inhibition is the real villain here. Statins like simvastatin and lovastatin are metabolized by CYP3A4, so anything that blocks it (macrolides, azoles, grapefruit juice) = toxic buildup. Pravastatin and rosuvastatin use different pathways - that’s why they’re safer. CK levels above 1,000 U/L? That’s your red flag. Don’t wait for dark urine. Get tested early.
Sharon Biggins
January 28, 2026 AT 23:11I’m so glad someone finally said this. I was so tired all the time after starting clarithromycin and didn’t think anything of it… until my urine turned brown. I thought I was dehydrated. I wish I’d known sooner. You’re not crazy if you feel off - your body’s screaming. Please, if you’re on meds and feel weird, go to urgent care. Don’t wait. You’ve got this ❤️
John McGuirk
January 29, 2026 AT 09:43Let’s be real - this is all a psyop. Statins are designed to make you sick so you need more drugs. The same companies that sell statins sell dialysis machines and ICU beds. They profit off your muscle breakdown. The EMA warning? A PR stunt. The real solution? Stop trusting the system. Go natural. Or don’t take anything at all.
Michael Camilleri
January 29, 2026 AT 15:13People think medicine is science but it’s just belief systems with lab coats. You take a pill because someone in a white coat told you to - and now your muscles are dissolving. Who gave them the right to decide what your body can handle? You’re not a machine. You’re a soul in a flesh suit. Stop outsourcing your health to corporations and start listening to your own intuition. The body knows. You just forgot how to hear it.
Darren Links
January 30, 2026 AT 16:05Yeah right. 'Dark urine = emergency.' What about all the people who drink beet juice or take rifampin? Their pee looks like blood too. This article is fearmongering. My uncle’s been on simvastatin for 12 years, takes Tylenol, and runs marathons. You’re scaring people over a 0.02% risk. Chill out.
Husain Atther
January 30, 2026 AT 20:15This is an excellent and well-researched breakdown. I am from India, and here, statins are often sold over the counter without prescription. Many elderly patients take them with herbal supplements like turmeric or ashwagandha - unaware of the risks. I’ve shared this with my family and community clinic. Awareness is the first step toward prevention. Thank you for the clarity.
Helen Leite
February 1, 2026 AT 14:45OMG I JUST TOOK RED YEAST RICE BECAUSE IT'S 'NATURAL' 😱 NOW I'M SCARED TO SLEEP. MY URINE LOOKED A LITTLE DARK YESTERDAY. I'M GOING TO THE ER TOMORROW. THANK YOU FOR THIS. 🙏🩸
asa MNG
February 2, 2026 AT 07:15bro i got a statin and a z pack last month and my thighs felt like concrete for 3 days but i thought it was just sore from lifting... turns out my CK was 6,400 and i almost lost a kidney lmao. docs dont care. i had to beg for the test. now i only take pravastatin and i dont trust anyone who says 'just take the pill' anymore. also i spelled a bunch of words wrong cause i was typing on my phone while crying in the ER