
When a patient skips a dose because the copay is too high, it’s not just a personal choice-it’s a system failure. Every year, cost-related nonadherence leads to 100,000 preventable deaths and $100-$300 billion in avoidable healthcare spending in the U.S. The fix isn’t complicated: lower the price of generic drugs, and patients actually take them.
Why Patients Skip Their Medications
It’s not laziness. It’s not forgetfulness. It’s money. A 2023 JAMA Network Open survey of over 2,100 adults found that 32.7% admitted to skipping doses, delaying fills, or not filling prescriptions at all because of cost. That’s more than one in three people. And when asked what would change their behavior, 78% said if they knew the real price upfront-especially if it was way higher than expected-they’d think twice before starting the treatment. The numbers don’t lie. For every $10 increase in out-of-pocket cost for a prescription, adherence drops by 2-4%. For diabetes drugs like GLP-1 agonists, that number jumps to 3.7%. That means a $50 copay could mean you’re 18% less likely to take your pills regularly than if it cost $10. And when patients don’t take their meds, they end up in the ER more often-5.2% more for diabetes patients alone.Generics Work Just as Well-And Cost Way Less
Generic drugs aren’t cheap because they’re low quality. They’re cheap because they don’t need to pay for ads, fancy packaging, or years of R&D. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they’re absorbed into the body at the same rate and to the same extent-within 80-125% of the brand. That’s not close. That’s clinically identical. And the price difference? 80-85% less. A brand-name statin like Crestor might cost $75 a month. The generic, rosuvastatin? $5. That’s not a discount. That’s a lifeline. A Reddit user named u/HeartHealthJourney shared how switching from brand to generic turned his adherence from missing 3-4 doses a week to perfect compliance for 11 months straight. Studies back this up. When Medicare Part D moved brand-name statins from tier 2 to tier 1 (lower cost), adherence jumped by 5.9%. In breast cancer treatment, patients on generic aromatase inhibitors had 73.1% adherence compared to 68.4% on brand names-even though both drugs worked the same. The only difference? Price.How Insurance Tiers Create Hidden Barriers
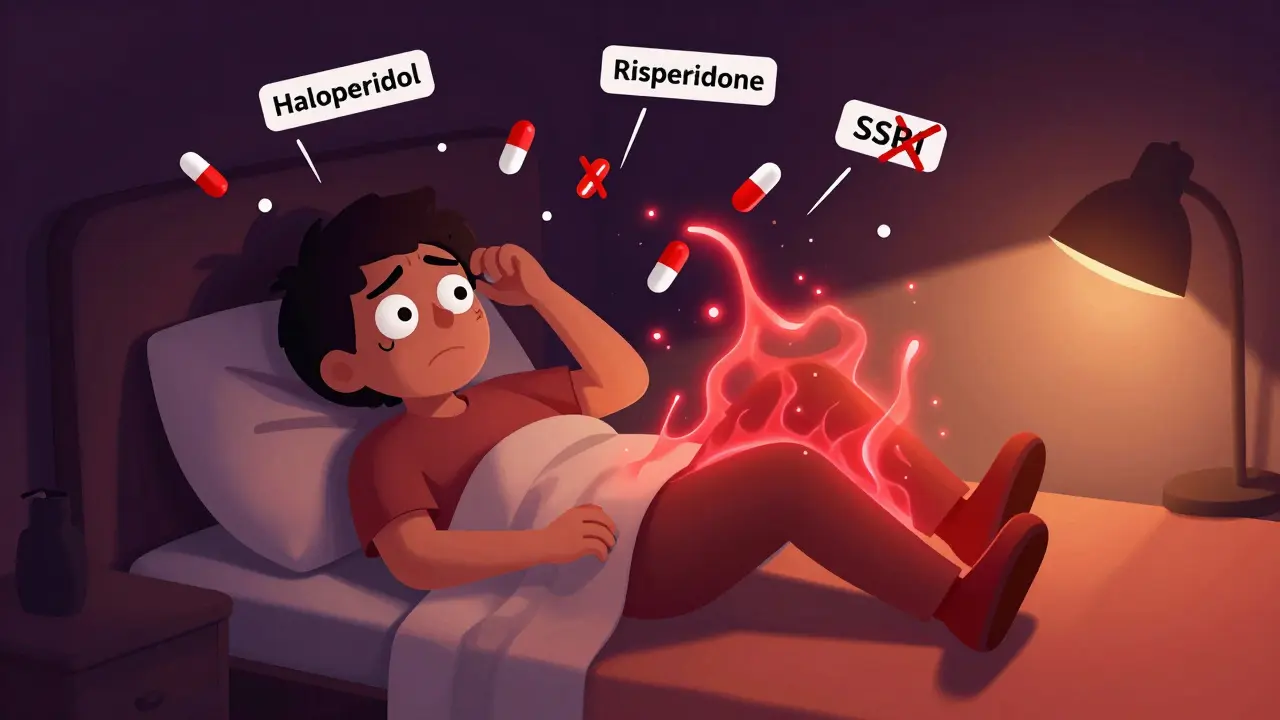
Insurance plans don’t just charge different prices-they create tiers that act like financial gates. Tier 1: generics, $10 copay. Tier 2: preferred brands, $40. Tier 3: non-preferred brands, $100+. That $90 difference isn’t just a number. It’s a decision point. For patients on fixed incomes, that’s not a choice between two meds. It’s a choice between taking their blood pressure pill or buying groceries. That’s why adherence plummets when a drug moves from tier 1 to tier 3. A 2022 review of 160 studies in the Journal of Managed Care & Specialty Pharmacy found that higher cost-sharing consistently led to lower adherence-especially for heart disease, diabetes, and mental health drugs. And it’s not just about the copay. Many patients don’t even know what their copay will be until they get to the pharmacy. That’s why real-time benefit tools (RTBTs) are changing the game. These tools show the exact price at the moment the doctor writes the prescription. Pilot programs using RTBTs saw adherence improve by 12-15%. Doctors who use them and actually talk to patients about cost? Patients are more likely to stick with the treatment.
What Happens When Patients Don’t Take Their Pills
Skipping meds doesn’t mean you’ll feel worse tomorrow. It means you’ll end up in the hospital six months from now. Medication nonadherence causes up to 50% of treatment failures. For heart failure patients, missing doses leads to more fluid buildup, more ER visits, more hospitalizations. For diabetics, it means higher A1c levels, more nerve damage, more kidney failure. For mental health, it means relapse, crisis, and sometimes suicide. The economic toll is massive. Every dollar spent on medication adherence saves $3-$10 in downstream care. A 2011 study showed that patients who took their meds as prescribed had 15-20% fewer hospital stays. That’s not a small gain. That’s a system-wide win.Policy Changes Are Making a Difference
The Inflation Reduction Act of 2022 capped insulin at $35 a month-a move that immediately helped millions. Starting in 2025, Medicare Part D will cap out-of-pocket drug spending at $2,000 a year. That’s huge. An estimated 1.4 million Medicare beneficiaries will benefit, with adherence expected to rise as a result. The FDA’s Generic Drug User Fee Amendments (GDUFA III), launched in 2023, is investing $1.1 billion to speed up generic approvals. By 2027, over 1,500 new generics could hit the market. More generics mean more competition, which means even lower prices. Meanwhile, programs like Magellan’s inforMED use AI to predict who’s at risk of skipping meds because of cost-and then intervene. They might switch the prescription to a cheaper alternative, offer a coupon, or connect the patient with financial aid. The result? A 2:1 return on investment and a 40% drop in care gaps.What Patients and Providers Can Do Today
You don’t need new laws to make a difference right now. If you’re a patient: Ask your pharmacist or doctor, “Is there a generic version?” Don’t assume the brand is better. Check GoodRx or SingleCare for real-time prices across pharmacies. Sometimes the cash price without insurance is lower than your copay. If you’re a provider: Use real-time benefit tools. Ask patients, “Can you afford this?” Don’t wait for them to admit they’re skipping doses. Make it part of the routine. Say, “I know meds can be expensive. Let’s find one that works for your budget.” And if you’re in charge of a clinic or pharmacy: Push for tiered formularies that put generics first. Train staff to explain that generics aren’t second-rate-they’re the same medicine, just without the marketing.
Myths That Still Hold People Back
There’s still a lot of misinformation. Some patients think generics are weaker. Others believe brand-name drugs work faster. Neither is true. The FDA’s “It’s Okay to Use Generics” campaign exists for a reason. People need to hear it from trusted sources. One study found that when patients were given a simple handout explaining bioequivalence, 68% were more willing to switch to a generic. Another myth: “My insurance won’t cover it.” That’s often false. Most plans cover generics at the lowest tier. If your plan says no, ask for a formulary exception. Many times, they’ll approve it if you explain the cost barrier.The Bigger Picture: Generics Are the Quiet Hero of Healthcare
Americans pay 256% more for brand-name drugs than people in other wealthy countries. Yet, 90% of prescriptions filled in the U.S. are generics-and they make up only 23% of total drug spending. That’s $643 billion saved between 2009 and 2019. We don’t talk about this enough. Generics aren’t just cheaper. They’re the reason millions of people with diabetes, high blood pressure, or depression can stay out of the hospital. They’re the reason families don’t have to choose between meds and rent. Lowering generic prices isn’t just good economics. It’s good medicine. It’s not about cutting corners. It’s about removing barriers to care.What’s Next?
The future is value-based insurance design-where copays are tied to how effective a drug is, not how expensive it is. For example, a high-value diabetes drug might have a $0 copay, while a low-value one costs more. Early pilots showed 18.3% higher adherence for high-value meds. We’re also seeing more telehealth platforms integrate pricing tools directly into virtual visits. Imagine your doctor prescribing a med-and right there on the screen, showing you the cheapest option, with a link to save it at your local pharmacy. The tools exist. The data is clear. The only thing missing is the will to use them.Do generic drugs work as well as brand-name drugs?
Yes. The FDA requires generics to contain the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they’re absorbed into the body at the same rate and to the same extent-within 80-125% of the brand. This is called bioequivalence. Generics are not weaker, slower, or less effective. They’re the same medicine, just without the marketing cost.
Why are generic drugs so much cheaper?
Brand-name drugs include the cost of research, development, clinical trials, and marketing-often over $2 billion to bring one drug to market. Generics don’t have to repeat those studies. Once a patent expires, other companies can make the same drug using the existing formula. That competition drives prices down-usually by 80-85%.
Does lowering the price of generics really improve adherence?
Yes, consistently. Studies show that for every $10 increase in out-of-pocket cost, adherence drops by 2-4%. When Medicare moved brand-name statins to lower-cost tiers, adherence rose by 5.9%. Patients on generic aromatase inhibitors for breast cancer had 73.1% adherence versus 68.4% on brand names. The pattern holds across diabetes, heart disease, and mental health conditions.
What should I do if I can’t afford my medication?
Ask your doctor if a generic version is available. Check GoodRx or SingleCare for the lowest cash price at nearby pharmacies. Ask about patient assistance programs from drug manufacturers. Some pharmacies offer $4 generic lists for common medications. Never skip doses without talking to your provider-they may be able to switch you to a cheaper alternative.
Why do some doctors still prescribe brand-name drugs?
Sometimes it’s habit. Sometimes they don’t know the price. Sometimes the patient asked for it. But many doctors still don’t have access to real-time pricing tools. When they do, they switch to generics 60-70% of the time. The problem isn’t doctors-it’s the system. Better tools, better data, and better conversations can fix that.
Are there cases where generics don’t work as well?
Rarely. For most medications, generics are equally effective. There are a few exceptions-like narrow-therapeutic-index drugs (e.g., warfarin, levothyroxine)-where tiny differences in absorption matter. But even then, switching between generics or from brand to generic is usually safe under medical supervision. The FDA monitors these closely. Less than 5% of studies suggest cost-adherence links are weaker in conditions like HIV, but even there, affordability still improves outcomes.




Bennett Ryynanen
December 31, 2025 AT 15:46Let me tell you something - I’ve seen people skip their blood pressure meds because they cost $40 a month. Then they end up in the ER with a stroke. This isn’t about ‘being responsible’ - it’s about capitalism being broken. Generics aren’t ‘cheaper’ - they’re the only thing keeping people alive. Stop acting like this is a moral issue. It’s a fucking supply chain failure.
Chandreson Chandreas
January 1, 2026 AT 20:51India makes 60% of the world’s generics 🌏💊. We don’t have fancy ads or CEOs on yachts. Just science. And yet, Americans pay 10x more? I get it - your system is built on profit, not patients. But hey, at least your pharmacy techs know your name. That’s something, right? 😅
Darren Pearson
January 3, 2026 AT 06:27One must acknowledge the profound economic inefficiencies inherent in the current pharmaceutical pricing architecture. The notion that bioequivalence equates to therapeutic equivalence is not universally empirically validated across all clinical contexts. One cannot conflate cost reduction with health equity without addressing systemic reimbursement fragmentation.
Hanna Spittel
January 3, 2026 AT 17:56Generics are just the first step. Big Pharma owns the FDA. They let generics in so they can patent the next ‘miracle’ drug that costs $1000/month. You think this is about saving lives? Nah. It’s about controlling the narrative. #PharmaControl
Brady K.
January 4, 2026 AT 11:22Oh wow, a 5.9% adherence increase when statins got cheaper? Groundbreaking. Meanwhile, the same people who scream about ‘personal responsibility’ are the ones who want to cut Medicaid. You want adherence? Pay people to take their meds. Or better yet - make healthcare a right, not a privilege. But sure, let’s keep pretending this is just about ‘copays’.
Kayla Kliphardt
January 5, 2026 AT 23:15I’ve always wondered - do pharmacists ever get trained to explain bioequivalence to patients? Or is that just assumed knowledge? I’ve never had someone sit down and say, ‘This is the same drug, just cheaper.’ Maybe that’s the real gap.
John Chapman
January 7, 2026 AT 23:06My grandma switched from brand to generic lisinopril and her BP dropped even better. She said, ‘I finally stopped choosing between pills and my cat’s food.’ 🐱❤️ This is the kind of change that doesn’t make headlines - but saves lives. We need more of this, not less.
Urvi Patel
January 9, 2026 AT 11:53Why are we even talking about generics when the real issue is that no one can afford insurance? You fix the system not the pill price. And stop pretending generics are magic. They’re just the bandaid on a bullet wound
anggit marga
January 9, 2026 AT 15:10USA thinks it invented medicine. Meanwhile China and India make the pills you buy. You pay 10x and still complain. This is what happens when you think your country is the center of the universe. Generics are not your enemy - your arrogance is
Joy Nickles
January 11, 2026 AT 13:16Okay so I just looked up my metformin… it’s $1.20 at Walmart? But my insurance copay is $25??? Who is running this system?? I’m not even mad… I’m just… confused? Like… who decided this was okay???
Harriet Hollingsworth
January 11, 2026 AT 16:00People who skip meds are lazy. They don’t care about their health. If they really wanted to live, they’d work harder. Why should I pay for someone else’s poor choices? This isn’t a right - it’s a privilege.
Deepika D
January 13, 2026 AT 06:55Let me tell you something - I used to work in a rural clinic in Tamil Nadu. We had patients who walked 15 kilometers to get their generic antihypertensives. They’d save for months. They’d trade eggs for pills. And they never missed a dose. Why? Because they knew it was their only shot. In the U.S., we have apps that show prices in real time, free coupons, and telehealth access - and people still skip meds because they’re ‘too busy’ or ‘don’t feel like it.’ It’s not the price. It’s the mindset. We need to teach people that taking your medicine isn’t a chore - it’s an act of self-respect.
Stewart Smith
January 14, 2026 AT 20:30So the FDA says generics are the same. But have you ever seen the fillers? Some generics use different dyes or binders. I had a friend who had a reaction to the red dye in one generic version of sertraline. Switched back to brand - problem gone. So yeah, ‘bioequivalent’ doesn’t always mean ‘identical experience.’