
Most people get vaccinated without a second thought. But for a tiny fraction, something unexpected happens: a reaction. Not the mild sore arm or low fever everyone expects - but something more serious. An itchy rash. Swelling. Trouble breathing. In the rarest cases, anaphylaxis. These events are terrifying to imagine, and they make headlines. But here’s the truth most people don’t hear: vaccine allergic reactions are extraordinarily rare. Far rarer than being struck by lightning. And we have systems in place to catch them, study them, and keep vaccines safe for everyone.
How Rare Are Allergic Reactions to Vaccines?
Let’s put numbers to fear. Across all vaccines given in the U.S., anaphylaxis - the most severe allergic reaction - happens about 1.3 times per million doses. That’s like flipping a coin 1 million times and getting heads on just one of them. For the mRNA COVID-19 vaccines, the rate went up slightly to about 5 to 11 cases per million doses. Still, that’s less than 0.001%. Compare that to the risk of a car crash on your way to the clinic, or even a severe reaction to a common antibiotic. The odds are overwhelmingly in your favor.
Most reactions happen fast. Eighty-six percent of anaphylaxis cases show up within 30 minutes of getting the shot. Over 70% happen in the first 15 minutes. That’s why clinics ask you to wait after vaccination. It’s not bureaucracy - it’s a safety net. If something happens, medical staff are right there with epinephrine, the one drug that can stop a life-threatening reaction in its tracks.
What Causes These Reactions?
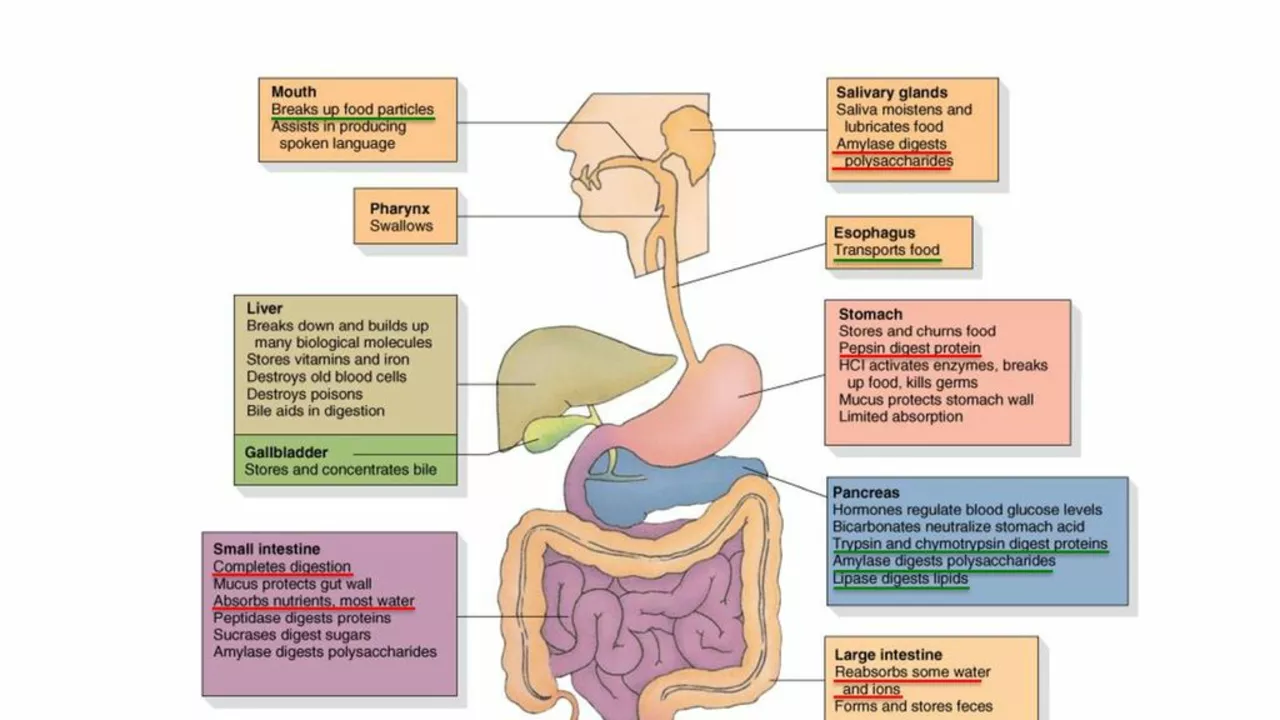
It’s not the virus or bacteria in the vaccine. Those are either dead, weakened, or just genetic instructions. The real culprits are the tiny bits added to help the vaccine work or stay stable. For years, people worried about egg proteins in flu shots. But research showed that even people with life-threatening egg allergies could safely get the flu vaccine. In fact, over 4,300 egg-allergic individuals received flu shots with no serious reactions - including 656 who had passed out from egg exposure before. Today, no special steps are needed.
Now, the focus has shifted to ingredients like polyethylene glycol (PEG) and polysorbate. These are in some mRNA vaccines and are known to trigger rare allergic responses. If someone has had a confirmed anaphylaxis to PEG before - say, from a CT scan contrast dye - they should talk to an allergist. But for the vast majority, even those with other allergies, PEG isn’t a problem. Yeast proteins? Only 15 possible cases ever reported in VAERS out of 180,000 allergy reports. Aluminum? It can cause a persistent lump under the skin, but not anaphylaxis.
Who’s Most Likely to Have a Reaction?
Women make up over 80% of reported allergic reactions after vaccines. The average age is around 40. That doesn’t mean women are more allergic - it likely reflects that more women get vaccinated, especially for flu, HPV, and COVID-19. People with a history of severe allergies - especially anaphylaxis to foods, insect stings, or medications - are at slightly higher risk. But even among them, the chance of a vaccine reaction remains extremely low.
Most reactions happen on the first dose, not the second. That suggests some people might already be sensitized to a component before ever getting the shot. It’s not the vaccine causing the allergy - it’s a hidden sensitivity that only shows up when the substance is injected.
How Do We Know When Something Goes Wrong?
There’s a quiet, powerful system working behind the scenes: VAERS - the Vaccine Adverse Event Reporting System. Run by the CDC and FDA since 1990, it’s not a database of proven side effects. It’s an early warning system. Anyone - a doctor, a patient, a pharmacist - can report anything unusual after vaccination. That includes rashes, dizziness, or even a headache. Most reports are unrelated to the vaccine. But when patterns emerge - like a spike in reactions after a specific batch - investigators dig in.
VAERS gets 30,000 to 50,000 reports a year. Allergic reactions make up a small slice. But because it’s open and public, it catches things no clinical trial ever could. For example, the first known anaphylaxis linked to the carrier protein CRM(197) in the pneumococcal vaccine was found through VAERS. A 12-month-old infant had a reaction - and that single report led to deeper research.
On top of that, the CDC uses v-safe, a smartphone tool that texts people after they get vaccinated. It asks how they’re feeling. Over 3.6 million people used it during the COVID-19 rollout. That real-time data helped confirm the anaphylaxis rate was still within expected limits - even with millions of doses given in record time.
What Happens If You Have a Reaction?
If you develop hives, swelling of the lips or tongue, wheezing, or a sudden drop in blood pressure within minutes of getting a shot - that’s an emergency. Epinephrine is given immediately. It works fast. In almost every case, people recover fully. No deaths from vaccine-related anaphylaxis have been confirmed in the U.S. since 2020, despite over a billion doses given.
Afterward, the reaction is reported to VAERS. If you’re worried about future vaccines, an allergist can help. They may do skin tests or blood tests to check for allergies to PEG, polysorbate, or other components. But here’s the key: even if you had a reaction, it doesn’t mean you can’t get vaccinated again. Many people who had anaphylaxis after the first dose of an mRNA vaccine were safely given a different type of vaccine later - like Novavax - without issue.

What About Egg Allergies? Still a Problem?
No. Not anymore.
For decades, people with egg allergies were told to avoid flu shots. That was because the virus was grown in chicken eggs. But modern purification removes nearly all egg protein. Studies showed no increased risk - even for those who had gone into anaphylaxis from eating eggs. The American Academy of Allergy, Asthma & Immunology changed its guidelines in 2011. Today, the CDC says: no special precautions. No allergy testing. No extended observation. Just give the shot. Same goes for MMR and varicella vaccines. Egg isn’t the threat it used to be.
What Do You Need to Do Before Getting Vaccinated?
Nothing - unless you’ve had a confirmed anaphylaxis to a vaccine component before. If you’ve ever had a severe reaction to PEG, polysorbate, or a prior dose of the same vaccine, talk to your doctor or an allergist. Bring your history. They’ll help you decide if it’s safe to proceed and which vaccine might be best.
For everyone else: show up. Get the shot. Stay for 15 minutes. Tell the nurse if you’ve ever had a serious allergic reaction to anything. That’s it. No need to avoid vaccines because of fear. The risk of getting sick from measles, flu, or COVID-19 is thousands of times higher than the risk of a severe reaction to the vaccine.
Why This Matters Beyond the Individual
When people skip vaccines because they’re scared of rare reactions, it doesn’t just hurt them. It hurts everyone. Outbreaks of measles, whooping cough, and other preventable diseases come back when vaccination rates drop. The systems we have - VAERS, v-safe, allergist evaluations - exist to make vaccines safer, not to scare people away. The data shows they work. We’ve gone from a 1976 flu vaccine linked to Guillain-Barré syndrome to a global network that monitors billions of doses annually. The science is better. The tools are sharper. The safety net is stronger than ever.
Getting vaccinated isn’t just about protecting yourself. It’s about protecting the person next to you - the baby too young for shots, the elderly with weak immune systems, the neighbor with cancer. The tiny risk of a reaction is far outweighed by the massive benefit of stopping deadly diseases in their tracks.




Ifeoma Ezeokoli
November 30, 2025 AT 05:18Okay but can we talk about how wild it is that we’re scared of a 0.001% chance when we hop in cars every day and don’t think twice? I got my third shot last week, waited my 15 minutes, and went to get bubble tea like normal. Life goes on. 🌸
Daniel Rod
December 1, 2025 AT 02:55It’s funny how fear loves to dress up as logic. We’ll panic over one in a million odds while ignoring the 1 in 50 chance of dying from the flu if we don’t get vaccinated. The real miracle isn’t the vaccine - it’s how we’ve built systems to catch the rarest of risks before they become tragedies. 🤝
gina rodriguez
December 1, 2025 AT 08:41I work in a clinic and I can tell you - the waiting room after vaccines is always so calm. People chat, scroll on their phones, sometimes cry a little from relief. We’ve had maybe two reactions in three years. The system works. You’re safer getting the shot than you are waiting in line for coffee.
Sue Barnes
December 2, 2025 AT 01:10VAERS? Please. It’s a dumping ground for every headache and hangnail since 2003. And don’t get me started on ‘no deaths since 2020’ - they’re not counting the ones who ‘died of complications’ two weeks later. They’re hiding the truth. 😒
jobin joshua
December 3, 2025 AT 09:50Bro I had a rash after my Pfizer and my cousin in Delhi said it’s because of the graphene oxide 😭 I’m scared now…
Sachin Agnihotri
December 3, 2025 AT 16:44Wait - graphene oxide?? That’s not even in the ingredients list… I mean, come on. PEG is the only known trigger, and even then, it’s like winning the lottery backwards. 🤷♂️
Diana Askew
December 3, 2025 AT 20:43They said the same thing about thimerosal. And now they’re putting microchips in the vials. You think they want you healthy? They want you docile. 🧪👁️
King Property
December 4, 2025 AT 07:52You people are idiots. If you think 5 per million is ‘rare,’ you’ve never seen a spreadsheet. The CDC hides the real numbers. I’ve got a cousin who died after the shot - they called it ‘cardiac arrest’ but it was the spike protein. I’ve got the autopsy. You’re being lied to.
Yash Hemrajani
December 5, 2025 AT 14:07Oh wow, so now we’re blaming PEG? Next you’ll say the real danger is the air inside the syringe. Look - if you’ve had anaphylaxis to PEG before, don’t get it. If not? Chill. Your fear is 1000x more dangerous than the vaccine.
Pawittar Singh
December 6, 2025 AT 08:40Hey, I’m a nurse in Mumbai and I’ve given over 5,000 shots since 2021. Only one reaction - and it was a lady who was terrified before even getting the needle. She cried, then hugged me after. We’re all scared of what we don’t understand. But knowledge? It’s the best vaccine. 💪❤️
Josh Evans
December 7, 2025 AT 20:55My grandma got her flu shot last week and said it felt like a tiny pinch. She’s 82. She’s still here. I think we’re overcomplicating this.
Allison Reed
December 8, 2025 AT 19:33The data is clear: vaccine-related anaphylaxis is rarer than being struck by lightning, and the systems monitoring it - VAERS, v-safe, allergist protocols - are among the most robust in medical history. Choosing not to vaccinate based on misinformation doesn’t make you brave. It makes you a liability to public health.