
More than cancer prevention is about catching tumors early-it’s about stopping them before they start. The truth is, we have more power over our cancer risk than most people realize. The World Health Organization says 30 to 40% of all cancers are preventable. That’s not a guess. That’s based on decades of data from millions of people. You don’t need a miracle drug or a genetic lottery win to lower your risk. You just need to change how you live.
What You Can Actually Do to Lower Your Cancer Risk
The biggest win? Quitting tobacco. Smoking causes 78% of lung cancers and contributes to 15-20% of all cancer deaths worldwide. It’s not just cigarettes. Vapes, cigars, chewing tobacco-they all raise your risk. If you’ve never smoked, don’t start. If you do smoke, quitting at any age cuts your risk. Five years after quitting, your risk of mouth, throat, and esophageal cancers drops by half. Ten years after quitting, your lung cancer risk is cut in half compared to someone still smoking.
Weight matters more than you think. Every 5-point increase in BMI above 25 raises your risk of postmenopausal breast cancer by 12%, kidney cancer by 10%, and colorectal cancer by 8%. You don’t need to become a bodybuilder or drop 50 pounds. Losing just 5-10% of your body weight can reduce inflammation linked to tumor growth by 25-30% within six months. That’s not theory-it’s what University of Arizona researchers saw in real patients.
Move your body. The goal isn’t to run marathons. It’s 150 minutes a week of brisk walking-that’s 30 minutes, five days a week. Or 75 minutes of running, cycling, or swimming. Mayo Clinic data shows this cuts colon cancer risk by 24% and breast cancer risk by 12-20%. If you sit all day, even a daily walk makes a difference. One study found people who took 10-minute walks after meals had better blood sugar control, which matters because high insulin levels fuel some cancers.
What You Eat (and What You Should Avoid)
Eat more plants. Aim for 2.5-3 cups of vegetables and 1.5-2 cups of fruit every day. That’s not a suggestion-it’s a proven shield. Cruciferous veggies like broccoli, cauliflower, and kale are linked to a 15-20% lower risk of prostate cancer, according to UC Davis Health’s 2024 review. Berries, citrus fruits, and leafy greens pack antioxidants and phytochemicals that help your cells repair DNA damage before it turns cancerous.
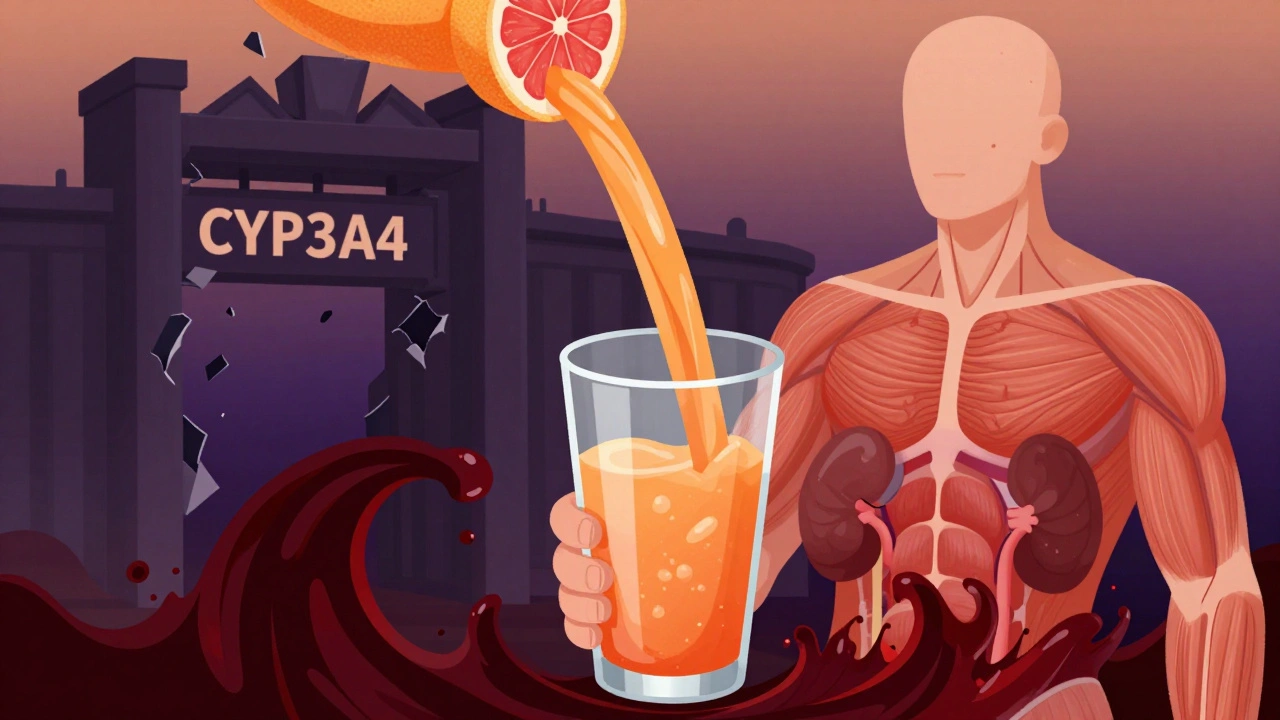
Limit processed meat. Bacon, hot dogs, deli meats, and sausages are classified as Group 1 carcinogens by the International Agency for Research on Cancer (IARC). That’s the same category as tobacco. The World Cancer Research Fund says avoid them entirely. The American Cancer Society says if you eat them, keep it under 18 ounces a week. Either way, cutting back helps. A 2023 study showed people who ate processed meat daily had a 20% higher risk of colorectal cancer than those who ate it once a month.
Alcohol isn’t harmless. Each extra drink a day raises breast cancer risk by 7-12%. For esophageal cancer, it’s 20-30% higher with just one daily drink. The guidelines are clear: men should have no more than two standard drinks (28g ethanol) a day. Women should stick to one (14g). That’s one 12-ounce beer, one 5-ounce glass of wine, or one 1.5-ounce shot of liquor. More than that? The risk climbs fast.
Sun Protection Isn’t Just About Wrinkles
UV radiation from the sun causes 90% of non-melanoma skin cancers and most melanomas. You don’t need to avoid the sun entirely, but you need to protect yourself. Use SPF 30+ broad-spectrum sunscreen every day-even when it’s cloudy. Reapply every two hours, or after swimming or sweating. Wear a wide-brimmed hat and UV-blocking sunglasses. Avoid direct sun between 10 a.m. and 4 p.m., when 80% of UV rays hit the earth.
Studies show consistent sunscreen use reduces melanoma risk by 50%. That’s not a small win. That’s life-changing. One woman in a Mayo Clinic study stopped getting new moles after just one year of daily sunscreen use. She didn’t change her diet or exercise. Just protected her skin. And her cancer risk dropped.
What Is Chemoprevention-and Who Should Consider It?
Chemoprevention means using drugs, vitamins, or natural substances to prevent cancer before it starts. It’s not for everyone. It’s for people at high risk-like those with a strong family history, genetic mutations (like BRCA1/2), or pre-cancerous conditions.
Examples include tamoxifen or raloxifene for women at high risk of breast cancer. These drugs can reduce risk by up to 50%. Aspirin, taken daily under a doctor’s care, has been shown to lower colorectal cancer risk by 20-40% over 10 years. But it’s not risk-free. Aspirin can cause stomach bleeding. Tamoxifen can increase blood clot risk. That’s why you need a doctor’s guidance. Chemoprevention isn’t a supplement you buy online. It’s a medical decision based on your personal risk profile.
Right now, only about 5-10% of people who could benefit from chemoprevention are even offered it. Most doctors don’t bring it up. But that’s changing. The American Society of Clinical Oncology launched ‘Prevention First’ in January 2024, training 5,000 oncologists to talk about prevention during routine visits. By 2025, that number will be in every clinic.
Why Most People Fail-And How to Succeed
People don’t fail because they’re lazy. They fail because they try to change everything at once. UCLA surveyed 1,200 people trying to prevent cancer. 68% said they couldn’t stick to exercise. Why? 74% said they didn’t have time. 52% said they couldn’t eat enough vegetables.
Here’s the fix: start with one thing. Pick the easiest change. Maybe it’s swapping soda for water. Or taking a 10-minute walk after dinner. Or putting sunscreen on your face every morning. Do that for a month. Then add another. UC Davis Health’s ‘Cultivating Health’ program paired activity tracking with group support. Participants hit 85% of their weekly goals. Control groups? Only 45%.
The American Cancer Society’s ‘3-2-1’ rule works because it’s simple: 30 minutes of activity daily, 2+ servings of vegetables at lunch or dinner, 1 hour less screen time. In community programs, 62% of people followed it. Those who set specific weekly goals? 87% stuck with it. Those with vague goals? Only 43%.
Small changes stick. Dr. Alpa Patel from the American Cancer Society says, ‘Small, sustainable changes yield better long-term results than drastic overhauls.’ Data shows 78% of people who focused on one habit kept it after 12 months. Only 32% kept multiple changes.
The Bigger Picture: Who’s Getting Left Behind?
Not everyone has equal access to prevention. CDC data shows only 31% of U.S. adults meet physical activity guidelines. Only 12% eat enough vegetables. Hispanic populations and people in the Southern U.S. have the lowest rates of healthy eating. Medicaid patients are less than half as likely to get lifestyle counseling as privately insured patients.
Employers are stepping in. 68% of Fortune 500 companies now offer cancer prevention programs. But participation? Only 42%. Why? Many programs are too complex. They offer nutritionists, fitness trackers, and apps-but don’t help people start small.
The real gap isn’t knowledge. Cancer Research UK found 64% know smoking causes cancer. But only 28% know obesity does. That’s the problem. We know the big dangers. We don’t know the quiet ones.
What’s Next? The Future of Prevention
The NIH is spending $287 million from 2024 to 2028 on lifestyle prevention research. They’re testing digital tools-apps that track food, movement, and sleep-to see what actually works. Results are due by December 2025.
Scientists are also testing personalized prevention. The NCI-MATCH trial is looking at whether your genes can tell you which diet lowers your cancer risk. Early data, expected in late 2025, could mean your next doctor’s visit includes a genetic report with a custom nutrition plan.
Harvard’s Walter Willett is tracking 120,000 people to see how combinations of habits-like diet + exercise + sleep-work together. Results come in late 2026. We might soon know that walking 30 minutes a day + eating broccoli + sleeping 7 hours cuts risk more than any one habit alone.
But here’s the bottom line: you don’t need to wait for a gene test or a fancy app. The tools are already here. Move more. Eat more plants. Avoid tobacco and processed meat. Limit alcohol. Protect your skin. These aren’t suggestions from a wellness influencer. They’re backed by science, decades of data, and millions of lives changed.
You can’t control everything. Genetics and environment play a role. But you control what you eat, how you move, and whether you light up a cigarette. That’s where the power lies.
Can lifestyle changes really prevent cancer?
Yes. The World Health Organization estimates 30-40% of all cancers are preventable through lifestyle choices. Studies show that following just three key recommendations-avoiding tobacco, staying at a healthy weight, and being physically active-can reduce cancer risk by 18-21% within five years. Even small changes, like losing 5-10% of body weight or walking 30 minutes a day, have measurable effects on cancer-related inflammation and hormone levels.
Is chemoprevention safe for everyone?
No. Chemoprevention-using drugs like tamoxifen or aspirin to lower cancer risk-is only recommended for people with high risk, such as those with genetic mutations or pre-cancerous conditions. These medications have side effects, including increased risk of blood clots or stomach bleeding. They should only be used under a doctor’s supervision after evaluating your personal risk profile. They are not meant for general population use.
How much physical activity do I need to reduce cancer risk?
The American Cancer Society recommends 150 minutes of moderate-intensity exercise (like brisk walking) or 75 minutes of vigorous activity (like running) per week. This reduces colon cancer risk by 24% and breast cancer risk by 12-20%. Even smaller amounts help-just 30 minutes a day, five days a week, makes a difference. The key is consistency, not intensity.
Does eating more vegetables really help prevent cancer?
Yes. Eating 2.5-3 cups of vegetables daily is linked to lower risks of several cancers, including colorectal and prostate cancer. Cruciferous vegetables like broccoli and cauliflower contain compounds that help detoxify carcinogens and reduce inflammation. A 2024 meta-analysis from UC Davis Health found a 15-20% lower prostate cancer risk in men who ate these vegetables regularly.
Why is processed meat considered a carcinogen?
Processed meats like bacon, sausage, and deli meats contain chemicals formed during curing, smoking, or heating that damage DNA in colon cells. The International Agency for Research on Cancer (IARC) classifies them as Group 1 carcinogens-the same category as tobacco and asbestos. Eating just 50 grams daily (about two slices of bacon) increases colorectal cancer risk by 18%. Avoiding them entirely is the safest choice.
Can I rely on supplements instead of eating whole foods?
No. Studies consistently show that cancer-preventing benefits come from whole foods, not pills. Antioxidants like vitamin C or E in supplement form haven’t been shown to reduce cancer risk and may even be harmful in high doses. The complex mix of fiber, phytochemicals, and nutrients in vegetables, fruits, and whole grains works together in ways supplements can’t replicate. Focus on food first.
How do I know if I’m at high risk for cancer?
You may be at higher risk if you have a strong family history of cancer, especially if multiple relatives had the same type before age 50, or if you carry known genetic mutations like BRCA1, BRCA2, or Lynch syndrome. Other factors include a history of pre-cancerous conditions (like colon polyps or Barrett’s esophagus), radiation exposure, or chronic inflammation. Talk to your doctor about genetic counseling or screening if any of these apply to you.





Marian Gilan
January 27, 2026 AT 05:59Conor Murphy
January 27, 2026 AT 19:09small steps, man. they add up.
Conor Flannelly
January 28, 2026 AT 12:35when you walk outside at dusk, when you eat something grown by hands you know, when you breathe without a screen between you and the air-you're not just preventing cancer. you're reclaiming your aliveness. the science just confirms what our ancestors knew instinctively.
Patrick Merrell
January 29, 2026 AT 04:58Geoff Miskinis
January 29, 2026 AT 20:16Moreover, the conflation of 'cancer risk reduction' with 'cancer prevention' is a semantic sleight-of-hand. You're not preventing cancer-you're attenuating probabilistic outcomes. This is not medicine. It's behavioral nudging dressed in lab coats.
Ryan W
January 30, 2026 AT 03:09Suresh Kumar Govindan
January 30, 2026 AT 07:39Ashley Karanja
January 31, 2026 AT 15:35But here's what I do: I put one apple in my kid's lunch every day. I take the stairs. I say no to soda. And I don't apologize for it. It's not about perfection. It's about showing up, even when the world tells you not to. That’s resistance. That’s power.
Uche Okoro
February 1, 2026 AT 06:32Faisal Mohamed
February 3, 2026 AT 01:10bella nash
February 3, 2026 AT 16:07