
When you take a blood thinner, you're trusting a medication to keep you safe from clots - but if you take too much, it can turn deadly. Blood thinners like warfarin, apixaban, rivaroxaban, and dabigatran prevent strokes and heart attacks by stopping blood from clotting too easily. But that same power makes them dangerous in overdose. Too much can cause uncontrolled internal bleeding, and the symptoms aren't always obvious until it's too late. Every hour counts. If you or someone you know has taken too much, knowing what to do can mean the difference between life and death.
What Happens When a Blood Thinner Overdose Occurs
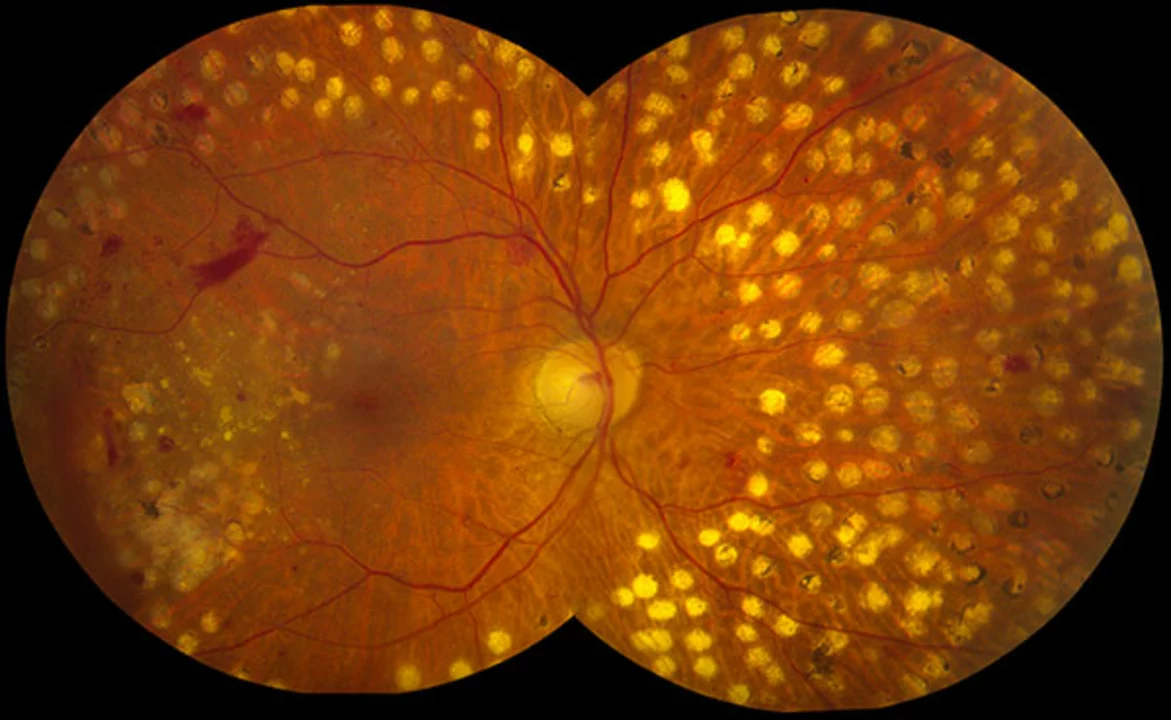
Blood thinners work by interfering with your body’s natural clotting system. Warfarin, the oldest and still widely used drug, blocks vitamin K, which your liver needs to make clotting factors. Without those factors, even a small bump can lead to serious bleeding inside your body. Newer drugs like apixaban and rivaroxaban block different parts of the clotting chain, but the result is the same: your blood can’t stop bleeding when it needs to. An overdose doesn’t always mean someone took ten pills at once. Sometimes it’s just one extra dose over several days, or a missed INR test that let levels creep too high. The danger builds slowly. For warfarin, your INR (a blood test that measures clotting time) might not spike until 12 to 24 hours after the overdose. By then, internal bleeding could already be underway. The most common signs of internal bleeding include:- Black, tarry, or bloody stools
- Pink, red, or dark brown urine
- Vomiting blood or material that looks like coffee grounds
- Unexplained bruising, especially large or spreading bruises
- Prolonged bleeding from minor cuts or gums
- Heavy menstrual bleeding that’s new or worse than usual
- Small red or purple dots under the skin (petechiae)
- Severe headache, dizziness, or confusion - possibly from brain bleeding
- Sharp pain in the abdomen, back, or chest
These aren’t just inconvenient symptoms. They’re red flags. A 2022 survey by the National Blood Clot Alliance found that 62% of patients ignored early signs, thinking it was something minor - like a stomach bug or a bruise from bumping into a door. By the time they went to the ER, many had lost so much blood their hemoglobin dropped below 7 g/dL. Normal is 12-16 g/dL. Below 7, your organs start shutting down.
What to Do Right Now If You Suspect an Overdose
If you notice any of these symptoms and you’re on a blood thinner, don’t wait. Don’t call your doctor’s office. Don’t check Google. Call 911 or go to the nearest emergency room immediately. Here’s what to do while you wait for help:- Stop taking any more of your blood thinner. Even one extra pill can push you over the edge.
- Do not take aspirin, ibuprofen, naproxen, or other NSAIDs. These drugs thin your blood further and make bleeding worse.
- Write down what you took, how much, and when. If you’re too sick to do it yourself, ask someone nearby. Emergency teams need this info fast.
- Stay calm and lie down. Elevate your legs slightly if you feel dizzy. Don’t stand up or move around unless absolutely necessary.
- Apply firm pressure to any external bleeding. Use a clean cloth or towel. Hold pressure for at least 10 minutes without lifting to check. If the cloth soaks through, add another layer on top - don’t remove the first one.
There’s no home remedy. No herbal tea. No ice pack. This is a medical emergency that requires hospital care.
How Hospitals Treat Blood Thinner Overdose
Treatment depends on what kind of blood thinner you took and how bad your INR or bleeding is.For warfarin overdose:
- If your INR is above 4.5 but you’re not bleeding: Doctors will give you oral vitamin K - usually 1 to 5 milligrams. This helps your body start making clotting factors again. It takes hours to work, so you’ll be monitored closely.
- If you’re actively bleeding: They’ll give you 4-factor Prothrombin Complex Concentrate (PCC) - a concentrated mix of clotting factors. It works in minutes. They’ll also give you 10 mg of IV vitamin K. In rare cases, if PCC isn’t available, they’ll use fresh frozen plasma (FFP), but that’s slower and riskier.
For DOACs (apixaban, rivaroxaban, dabigatran):
- If you took dabigatran (Pradaxa): There’s a specific antidote called idarucizumab. It reverses the drug in under 5 minutes. It costs around $3,500-$5,000 per dose, but it’s life-saving.
- If you took apixaban or rivaroxaban: Andexanet alfa is the antidote. It’s given as an IV infusion and starts working within minutes.
- If you’re not bleeding and the drug was taken within the last hour: Doctors might give you activated charcoal to stop further absorption - but only if you’re awake and able to swallow.
These reversal agents are not available everywhere. Smaller hospitals may not stock them. That’s why getting to a major ER quickly matters - time is what you’re fighting against.
Why People Delay - and Why That’s Deadly
Many patients don’t realize how fast things can go wrong. A 2022 study in the Blood Journal found that 28% of people waited more than 12 hours after symptoms started before seeking help. Why? Because they thought:- “It’s just a nosebleed - I’ve had them before.”
- “My stool is dark - must be from the iron pills.”
- “I’m tired because I didn’t sleep well.”
But internal bleeding doesn’t wait. A slow bleed into your abdomen or brain can go unnoticed for hours while your body quietly loses blood. By the time you feel weak or dizzy, you may have already lost 30% of your total blood volume. That’s when your heart starts racing, your skin turns pale, and your blood pressure crashes.
One Reddit user, u/WarfarinWarrior, shared his story: “I thought my dark stools were from something I ate. By the time I got to the ER, my hemoglobin was 6.2. My INR was 8.7. I almost died.” He spent 5 days in the hospital. His recovery took months.
On the flip side, patients who went to the ER within 2 hours of noticing symptoms had a 97% survival rate. Delay past 6 hours? Survival drops to 76%.
How to Prevent an Overdose in the First Place
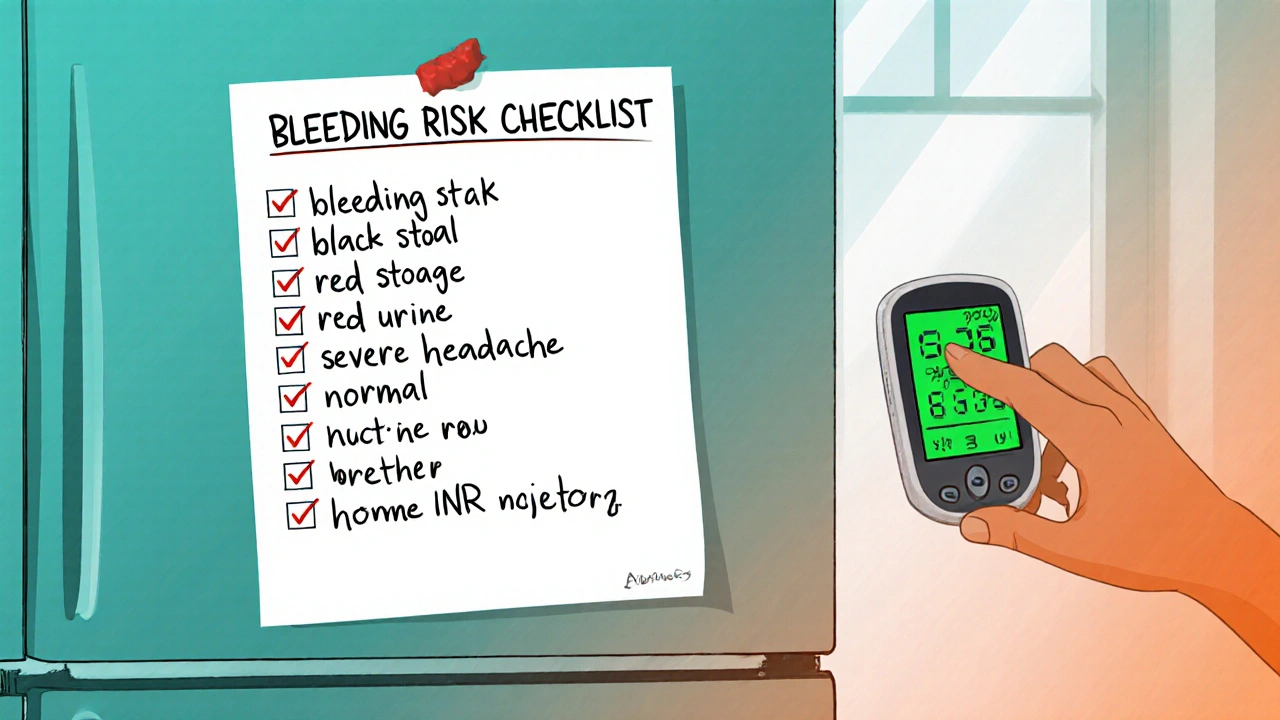
Prevention is the best treatment. Here’s how to stay safe:- Get your INR checked regularly. If you’re on warfarin, your doctor should test your INR every 1 to 4 weeks, depending on stability. If your INR is above 3.0 (or 3.5 if you have a mechanical heart valve), your dose may need adjusting.
- Use a pill organizer. Many overdoses happen because people forget if they already took their dose. A simple weekly pill box with labeled compartments prevents double-dosing.
- Keep a bleeding risk checklist. Post it on your fridge. Include: nosebleeds over 10 minutes, unexplained bruising, red urine, black stools, severe headaches. If any appear - go to the ER.
- Know your drugs. If you take a DOAC, know its name and when you last took it. Keep a card in your wallet with the drug name, dose, and your doctor’s number.
- Avoid alcohol and certain supplements. Alcohol increases bleeding risk. So do fish oil, garlic, ginkgo, and vitamin E in high doses.
- Ask about point-of-care INR monitors. These small devices let you test your INR at home. Studies show they reduce major bleeding by 34%. They cost $200-$300 - and many insurance plans cover them.
What’s Next for Blood Thinner Safety
New treatments are on the horizon. Ciraparantag, a universal reversal agent being tested in Phase III trials, could reverse any blood thinner - warfarin, DOACs, even heparin - within minutes. It’s not approved yet, but early results are promising.Meanwhile, the FDA requires all blood thinner packaging to carry a boxed warning about bleeding risks. Doctors are now required to use tools like the HAS-BLED score to assess your risk before prescribing - checking for high blood pressure, kidney or liver problems, past bleeding, age over 65, and other drugs you take.
But no system is perfect. The CDC says anticoagulant errors are the second most common serious medication mistake in adults over 65. That’s why your awareness matters most.
Can I just stop taking my blood thinner if I’m worried about bleeding?
No. Stopping your blood thinner suddenly can cause a clot to form, leading to stroke, heart attack, or pulmonary embolism. Never stop or change your dose without talking to your doctor. If you’re worried about bleeding, ask about your INR, your bleeding risk score, or whether a different medication might be safer for you.
How long does it take for a blood thinner to leave your system?
It varies. Warfarin lasts 2 to 5 days after your last dose because of its long half-life. DOACs like apixaban and rivaroxaban clear faster - usually within 12 to 24 hours. But even after the drug is gone, your body may still be vulnerable to bleeding for a few days. That’s why you need to stay alert for symptoms even after you’ve missed a dose or stopped taking it.
Is there a way to test for a blood thinner overdose at home?
Only if you have a home INR monitor - these devices let you check your clotting time like a glucose meter. But they don’t tell you if you’re bleeding internally. Symptoms like black stool, blood in urine, or severe headache are your real warning signs. If you have them, go to the ER - don’t wait for a test result.
Can I take painkillers if I’m on a blood thinner?
Avoid NSAIDs like ibuprofen, naproxen, and aspirin - they increase bleeding risk. Acetaminophen (Tylenol) is generally safe in standard doses, but never exceed 3,000 mg per day. Always check with your doctor before taking any new medication, even over-the-counter ones.
What should I do if I accidentally take two doses?
Call your doctor or pharmacist right away. If it’s after hours, go to the ER. Don’t wait for symptoms. If you took a DOAC, they may give you activated charcoal if it’s been less than an hour. If you’re on warfarin, they’ll likely schedule an INR test within 24 hours. Either way, don’t take another dose until you’ve been cleared.




Rodney Keats
November 17, 2025 AT 13:31Oh wow, so if I take my blood thinner and then accidentally eat a whole pack of gummy worms, does that count as an overdose? 🤔 Just kidding... unless? I mean, I’ve definitely forgotten if I took mine and then took another one because I was ‘so sure I didn’t.’ Thanks for the reminder that my body is basically a leaking balloon held together by hope and vitamin K.
Laura-Jade Vaughan
November 18, 2025 AT 07:30Wow. This is *so* important. 💔 I just had my aunt hospitalized last month because she thought ‘dark stool = just coffee’ 😭 And honestly? This post should be mandatory reading for every person over 50. Like, print it out. Tape it to the fridge. Put it in your wallet next to your insurance card. 🩸🩹 #BloodThinnerAwareness #DontWaitForTheScream
Jennifer Stephenson
November 19, 2025 AT 01:57Take medication as prescribed. Know the signs. Go to the hospital if unsure.
Segun Kareem
November 19, 2025 AT 09:21Life is a delicate dance between science and surrender. We take these pills to live longer - but we forget that survival isn’t just about the drug. It’s about awareness. It’s about listening to your body before it screams. This isn’t fear-mongering. This is love in the form of a warning. Share this. Save someone. The quietest symptoms are the loudest truths.
Philip Rindom
November 20, 2025 AT 00:18Honestly? I thought I was being smart by skipping my INR test because ‘I felt fine.’ Turns out, ‘feeling fine’ is the #1 reason people end up in the ER with internal bleeding. Thanks for the gut-check. I’ve scheduled my test now. Also, I’m getting that home monitor. Worth every penny.
Parv Trivedi
November 20, 2025 AT 02:19Very informative and well-structured. I have been on apixaban for 3 years now. I never realized how fast things can escalate. I now keep a small card in my wallet with the drug name, emergency number, and the list of symptoms. I also told my entire family about it. Knowledge is protection. Thank you for sharing this.
Willie Randle
November 20, 2025 AT 18:13There is a critical gap in public health education around anticoagulants. This post correctly identifies that symptom recognition - not just dosage compliance - is the linchpin of patient safety. The CDC’s data on anticoagulant errors being the second most common serious medication mistake in adults over 65 is not just a statistic - it is a systemic failure. Healthcare providers must prioritize patient education as rigorously as they do prescription writing.
Connor Moizer
November 21, 2025 AT 00:11You people are still reading this like it’s a self-help book? Get real. If you’re on a blood thinner and you’re not using a pill organizer, you’re playing Russian roulette with your organs. I’ve seen guys die because they ‘thought they were fine.’ Stop being lazy. Stop being denial-prone. Get the monitor. Write the checklist. Tell your damn family. This isn’t optional. Your life isn’t a suggestion.
kanishetti anusha
November 22, 2025 AT 15:01I’m so glad this was posted. My mom is on warfarin and I’ve been trying to explain this to her for months. She thinks ‘if I don’t feel sick, I’m fine.’ I’m printing this out and putting it on her fridge. She’s stubborn, but maybe seeing it in writing will help. Thank you for making this so clear. I’m sharing this with everyone I know.