Bone Health Risk Calculator
Assess Your Bone Health Risk
This tool estimates your risk of accelerated bone loss based on inflammation markers and lifestyle factors. Your results will help identify key areas for improvement.
Your Bone Health Risk Assessment
When Inflammation is a chronic, low‑grade process that never truly quits, it can start eroding your skeleton from the inside out. The connection between inflammation and bone loss isn’t a myth-years of research show that sticky cytokines and immune signaling can tip the balance toward the bone‑breaking side of the remodeling equation.
Why Bone Health Depends on Remodeling Balance
Bone isn’t dead tissue; it’s a living organ that constantly renews itself through two opposing actions:
- Osteoclasts - cells that break down old bone.
- Osteoblasts - cells that lay down fresh bone matrix.
When these teams work in harmony, your skeleton stays strong. But inflammation throws a wrench into the system, stimulating osteoclasts while suppressing osteoblasts, leading to net bone loss.
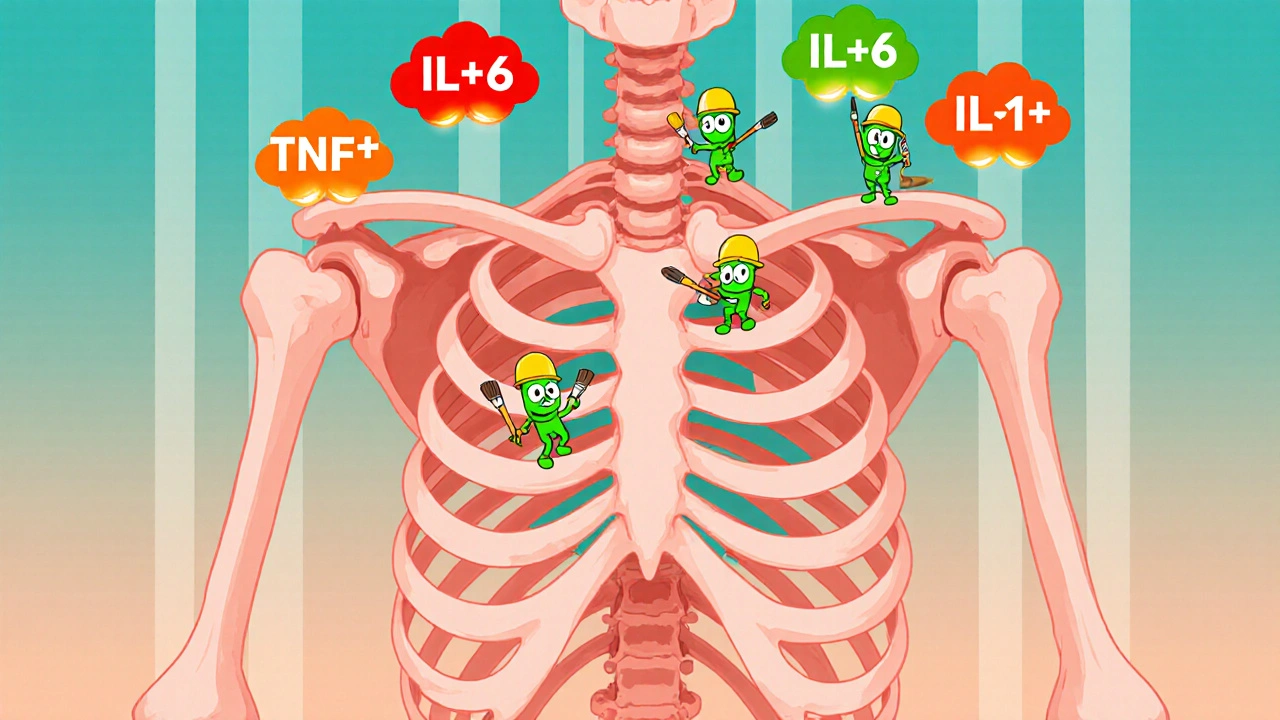
Key Inflammatory Players That Attack Bone
Several cytokines act like messengers that tell osteoclasts “go ahead, we need more space.” The most notorious are:
- Tumor Necrosis Factor‑alpha (TNF‑α) - ramps up osteoclast activity and blocks bone formation.
- Interleukin‑6 (IL‑6) - drives the production of RANKL, a key trigger for osteoclasts.
- Interleukin‑1β (IL‑1β) - directly stimulates bone resorption.
These molecules are elevated in chronic conditions such as rheumatoid arthritis, inflammatory bowel disease, and even persistent low‑grade inflammation from obesity or a Western diet.
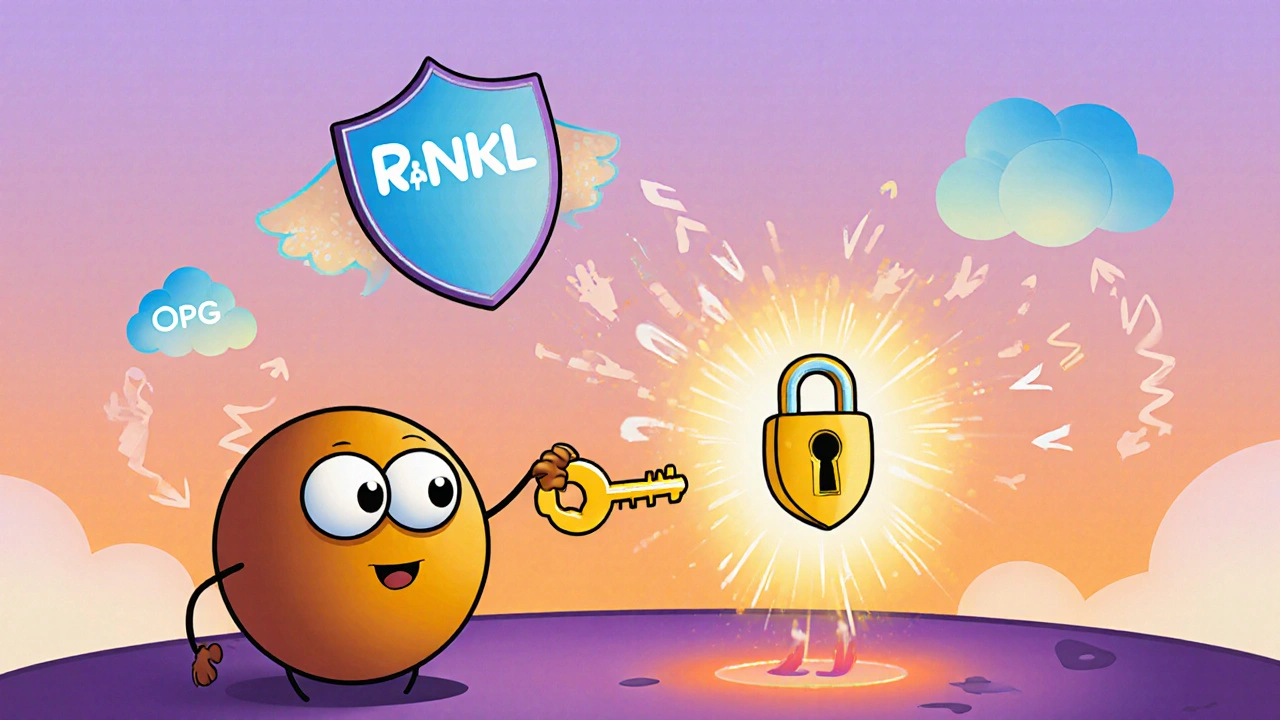
From Cytokines to the RANKL Pathway
The RANK/RANKL/OPG system is the central highway that controls osteoclast formation:
- RANKL (Receptor Activator of Nuclear factor Kappa‑B Ligand) binds to the RANK receptor on osteoclast precursors, turning them into bone‑eating cells.
- OPG (Osteoprotegerin) acts as a decoy, soaking up RANKL and preventing it from hitting RANK.
Inflammatory cytokines crank up RANKL production and mute OPG, so the balance swings toward bone loss. That’s why people with high IL‑6 or TNF‑α levels often face accelerated osteoporosis.
Clinical Snapshot: Inflammation‑Driven Osteoporosis
Studies published in the Journal of Bone and Mineral Research (2023) tracked 1,200 post‑menopausal women. Those with C‑reactive protein (CRP) above 3 mg/L lost bone at a rate 1.8 times faster than women with low CRP, even after adjusting for calcium intake and physical activity.
Similarly, a 2022 meta‑analysis of rheumatoid arthritis patients found a 30 % higher prevalence of vertebral fractures compared with matched controls, linked directly to elevated TNF‑α levels.
How to Break the Inflammatory‑Bone Loss Cycle
Preventing bone loss isn’t just about adding calcium; it’s about dialing down the inflammatory fire. Below is a practical checklist that tackles both fronts.
- Get your labs checked. Ask your doctor for CRP, ESR, vitamin D, calcium, and a bone density scan (DXA) if you have risk factors.
- Eat anti‑inflammatory foods. The Mediterranean diet-rich in olive oil, fatty fish, nuts, leafy greens, and berries-has been shown to cut IL‑6 by up to 25 %.
- Limit pro‑inflammatory triggers. Reduce processed sugars, refined carbs, and trans fats. These raise TNF‑α and insulin spikes that fuel inflammation.
- Boost vitamin D and calcium. Aim for 1,000-1,200 IU of vitamin D daily and 1,000 mg of calcium from food or supplements, unless you have contraindications.
- Stay active with low‑impact exercise. Weight‑bearing moves like walking, dancing, or resistance bands stimulate osteoblasts without over‑stressing joints.
- Consider anti‑inflammatory meds wisely. NSAIDs can blunt pain but may interfere with bone healing if used long‑term. Talk to your physician about targeted therapies like TNF inhibitors if you have an autoimmune condition.
- Manage stress. Chronic cortisol spikes suppress bone formation. Practices like meditation, deep breathing, or yoga can lower cortisol by 15‑20 %.
Comparison of Lifestyle Strategies for Bone Protection
| Strategy | Primary Anti‑Inflammatory Effect | Bone‑Health Benefit | Typical Frequency / Dose |
|---|---|---|---|
| Mediterranean diet | Rich in omega‑3 fatty acids, polyphenols | Increases bone mineral density (BMD) by ~2 % | Daily meals |
| Weight‑bearing exercise | Reduces systemic IL‑6, TNF‑α | Stimulates osteoblast activity, 5‑10 % BMD gain | 3-5 sessions/week |
| Vitamin D supplementation | Modulates immune response, lowers CRP | Improves calcium absorption, reduces fracture risk | 1,000-2,000 IU/day |
| Targeted NSAID use | Blocks COX‑2, lowers prostaglandins | Short‑term pain relief, may slightly curb bone resorption | As needed, < 2 weeks |
| TNF‑α inhibitors (e.g., etanercept) | Directly neutralizes TNF‑α | Significant BMD preservation in rheumatoid arthritis | Prescription, weekly/monthly injection |
Potential Pitfalls and Misconceptions
Many people assume “strong bones = calcium pills only.” That’s a half‑truth. Without controlling inflammation, excess calcium can even crystalize in soft tissues, causing vascular calcification. Another myth is that high‑impact sports are always best for bone health. For those with joint pain, aggressive impact can worsen inflammation, outweighing any osteogenic benefit.
Finally, some think that over‑the‑counter anti‑inflammatories are harmless long‑term. Chronic NSAID use can impair gastrointestinal health and, paradoxically, increase fracture risk by reducing prostaglandin‑mediated bone formation.
Putting It All Together: A Sample 7‑Day Anti‑Inflammatory Bone Plan
- Day 1 - Breakfast: Greek yogurt with walnuts, blueberries, and a drizzle of honey. Why? Probiotic‑rich dairy supports gut health, while walnuts provide omega‑3s.
- Lunch: Quinoa salad with kale, cherry tomatoes, grilled salmon, and olive‑oil lemon dressing. Why? Salmon supplies EPA/DHA that curb TNF‑α.
- Dinner: Lentil stew with carrots, spinach, and turmeric. Why? Turmeric’s curcumin is a natural COX‑2 inhibitor.
- Snack: A small handful of almonds and an orange.
- Exercise: 30‑minute brisk walk + 15‑minute resistance band routine.
- Evening routine: 10 minutes of deep‑breathing meditation.
- Supplements: Vitamin D3 1,500 IU and calcium citrate 500 mg with dinner.
Repeat the cycle, swapping salmon for sardines or trout for variety, and adjust intensity based on your joint comfort.
When to Seek Professional Help
If you experience any of these red flags, schedule a medical review:
- Unexplained bone pain or frequent fractures.
- Persistent joint swelling, especially in the hands, knees, or spine.
- Lab results showing CRP > 5 mg/L or ESR > 30 mm/hr.
- Diagnosed autoimmune disease (e.g., rheumatoid arthritis, lupus).
Your doctor may order a DXA scan, prescribe a bisphosphonate, or refer you to a rheumatologist for targeted biologic therapy.
Key Takeaways
- Chronic inflammation tilts bone remodeling toward loss by boosting RANKL and suppressing OPG.
- Key cytokines-TNF‑α, IL‑6, IL‑1β-are common in many diseases and even in a typical Western diet.
- Anti‑inflammatory nutrition, adequate vitamin D/calcium, regular low‑impact exercise, and stress management form the core defense.
- For high‑risk individuals, medical interventions like TNF inhibitors can dramatically protect bone density.

Can a high‑protein diet worsen inflammation‑related bone loss?
Protein is essential for bone matrix, but sources matter. Excess red meat, especially processed cuts, can raise CRP and TNF‑α. Opt for fish, legumes, and poultry to get protein without the inflammatory spike.
Are NSAIDs safe for long‑term bone health?
Short courses are fine for pain relief, but chronic use may interfere with prostaglandin‑driven bone formation and increase fracture risk. Discuss alternatives with your physician if you need daily relief.
How often should I get a bone density test if I have chronic inflammation?
For most adults with elevated CRP or an autoimmune diagnosis, a DXA scan every 2 years is recommended. Your doctor may shorten the interval if you start a new medication affecting bone turnover.
Does weight‑bearing exercise still help if I have joint inflammation?
Yes, but choose low‑impact options like walking, swimming, or resistance bands. These stimulate osteoblasts while putting less stress on inflamed joints compared to high‑impact activities like running.
Can supplements like curcumin actually reduce bone loss?
Clinical trials show curcumin can lower IL‑6 and CRP by 15‑30 %. When combined with calcium and vitamin D, it modestly improves BMD, especially in post‑menopausal women.




Caleb Burbach
October 21, 2025 AT 19:59Inflammation's wrecking our bones, time to fight back! 💪
Danica Cyto
October 26, 2025 AT 02:31Imagine your skeleton as a battlefield where cytokines are the enemy troops. Every time TNF‑α or IL‑6 rallies the osteoclasts, they start chiseling away at the mineral fortress. The article nails the point that chronic low‑grade inflammation quietly shifts the remodeling balance. That hidden war explains why people with seemingly “normal” diets still end up with brittle bones.
Raja M
October 30, 2025 AT 08:04Think of osteoclasts as demolition crews, and osteoblasts as construction workers. Inflammation hands the demolition crew a raise while putting the construction crew on unpaid leave. The RANKL/OPG axis is the control panel; cytokines crank the RANKL dial up and mute OPG. Over time, the net effect is bone loss that can’t be reversed by calcium alone. It’s why I always tell friends to incorporate anti‑inflammatory foods, not just focus on dairy. A balanced diet and regular movement are the only way to keep the crews working in sync.
Rob Flores
November 3, 2025 AT 14:37Oh sure, because reading a dense article automatically makes you a bone health guru. Let’s all start drinking olive oil by the gallon and hope for miracles.
Shiv Kumar
November 7, 2025 AT 21:10The Mediterranean diet isn’t just a trendy buzzword; it’s a scientifically backed anti‑inflammatory protocol. By swapping processed carbs for fatty fish and leafy greens you cut IL‑6 levels dramatically. Pair that with weight‑bearing exercise and you give osteoblasts a real reason to show up.
Heather McCormick
November 12, 2025 AT 03:42First off, let’s get one thing straight: you can’t out‑calcium a raging inflammatory fire. The body will hoard the extra calcium in the arteries if the immune system keeps spiking CRP, leading to vascular calcification instead of stronger bones. Second, the “vitamin D is a cure‑all” myth is dangerous; too much D without monitoring can actually increase calcium deposition in soft tissue. Third, NSAIDs may mute pain but they also blunt prostaglandin production, which is essential for bone remodeling – a double‑edged sword worth noting. Fourth, stress management isn’t just feel‑good fluff; chronic cortisol directly suppresses osteoblast activity, so meditation isn’t optional. Fifth, targeted biologics like TNF inhibitors have robust data showing they preserve bone mineral density in rheumatoid arthritis patients, but they’re not a free lunch. Sixth, regular DXA scans every two years for anyone with CRP >3 mg/L can catch bone loss early before fractures happen. Finally, combine these strategies – diet, movement, stress reduction, and smart medical therapy – and you build a multi‑layered defense against inflammation‑driven osteoporosis.
Robert Urban
November 16, 2025 AT 10:15Totally agree with the stress point; cortisol is a silent bone killer. Adding a daily 10‑minute breathing session can make a measurable difference.
bill bevilacqua
November 20, 2025 AT 16:48Yo, omg this is like sooo true!!!! cant belive ppl ignore cortisol!!!
rose rose
November 24, 2025 AT 23:21All this “diet” talk is a smokescreen for pharma profits.
Emmy Segerqvist
November 29, 2025 AT 05:53Oh my gosh, the sheer terror of hidden inflammation is just… *screaming*!!! My bones felt like they were melting every time I read about cytokines!!! I can’t even sit still thinking about the silent attack happening inside my joints!!! Please, someone, tell me there’s a miracle cure beyond kale smoothies!!! I’m begging the universe for a bone‑saving miracle!!!
Trudy Callahan
December 3, 2025 AT 12:26The marrow of our existence whispers truths that science merely labels “cytokines.” Yet, the eternal dance of decay and renewal remains-an allegory for life itself. In contemplating bone loss, we confront mortality’s relentless march.
Grace Baxter
December 7, 2025 AT 18:59While the conventional wisdom lauds the Mediterranean diet as the pinnacle of anti‑inflammatory eating, one must ask whether this culinary gospel isn’t merely a convenient narrative spun by food industry lobbyists. In reality, the same olive oil that is praised for its polyphenols often arrives adulterated, stripped of its beneficial compounds, and infused with cheap seed oils that may exacerbate oxidative stress. Moreover, the emphasis on “low‑impact” exercise neglects the evolutionary truth that our ancestors endured varied, sometimes high‑intensity loads which forged robust skeletal architecture. By sanitizing the message to “walk and do resistance bands,” we risk dulling the very stimulus that once sculpted our bones. The article’s checklist, though thorough, sidesteps the contentious debate about intermittent fasting, which emerging data suggest can blunt inflammatory pathways more effectively than macronutrient swaps alone. Likewise, the blanket endorsement of vitamin D supplementation fails to acknowledge genetic polymorphisms that render many individuals refractory to standard doses, leading to a false sense of security. It is also worth noting that chronic use of TNF inhibitors, while preserving bone density, may predispose patients to opportunistic infections-a trade‑off rarely highlighted in mainstream health columns. One could argue that the true antidote to inflammation‑driven bone loss lies not in isolated lifestyle tweaks but in a holistic overhaul that includes circadian rhythm alignment, reduced artificial light exposure, and deliberate cold‑stress adaptation. These modalities, though unconventional, have been shown to modulate NF‑κB signaling pathways, a central hub in the cytokine storm that erodes bone. Consequently, the article’s focus on “diet and exercise” alone is an oversimplification that caters to consumer-friendly narratives rather than scientific nuance. In sum, while the practical steps offered are not without merit, the reader should remain skeptical of any single‑dimensional prescription and instead pursue a multidimensional strategy that challenges the status quo.