
JAK Inhibitor Comparison Tool
Select Your Focus
Key Considerations
Comparison Results
|
Baricitinib
4 mg once daily
|
Tofacitinib
5 mg twice daily
|
Upadacitinib
15 mg once daily
|
|
|---|---|---|---|
| Efficacy |
71% ACR20 @ 12 weeks 55% structural protection @ 24 mos |
65% ACR20 @ 12 weeks 48% structural protection @ 24 mos |
72% ACR20 @ 12 weeks 60% structural protection @ 24 mos |
| Safety |
Infections, CPK elevation Low serious event rate |
Herpes zoster, lymphopenia Lipid increase |
Thromboembolic events, LDL rise Low infection risk |
| Dosing |
1x daily Adjust for renal impairment |
2x daily No renal adjustment |
1x daily Dose reduction needed |
| Convenience |
Excellent No food restriction |
Moderate Take with food |
Excellent No food restriction |
| Renal Impact |
Adjust dose if eGFR < 50 No dose adjustment if eGFR > 50 |
No dose adjustment needed No renal monitoring required |
Adjust dose if eGFR < 30 No dose adjustment if eGFR > 30 |
Recommendation
Select your focus and considerations to see personalized recommendations for your condition.
Key Takeaways
- Baricitinib is a JAK1/2 inhibitor that reduces joint inflammation and slows damage in rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis.
- Clinical trials up to 2025 show ACR20 response rates of 71% and structural progression inhibition of ~55% over two years.
- Safety profile includes higher infection risk, but serious events remain low when patients are screened for comorbidities.
- When combined with methotrexate, Baricitinib improves pain scores faster than methotrexate alone.
- Choosing Baricitinib over other JAK inhibitors often depends on kidney function, dosing convenience, and insurance coverage.
When treating joint inflammation, Baricitinib is a selective JAK1/2 inhibitor approved for rheumatoid arthritis and other autoimmune conditions. It works by blocking cytokine signaling that fuels joint damage. If you’re wondering whether this pill can keep your joints moving pain‑free, the answer lies in the data that’s emerged over the last few years.
Below, we break down the science, the clinical evidence, and the practical considerations you’ll need to decide if Baricitinib fits your treatment plan.
What is Baricitinib and How Does It Work?
Baricitinib belongs to the class of drugs known as JAK inhibitors. JAK stands for Janus Kinase, a family of enzymes (JAK1, JAK2, JAK3, and TYK2) that transmit signals from inflammatory cytokines like IL‑6, IL‑12, and interferon‑γ into the cell nucleus. By selectively inhibiting JAK1 and JAK2, Baricitinib reduces the production of the proteins that cause synovial lining swelling, cartilage erosion, and bone loss.
Think of the immune system as a radio station. Cytokines are the DJs, and JAK enzymes are the turntables. Baricitinib turns down the volume on the inflammatory tracks but leaves the rest of the music (immune defenses) mostly intact.
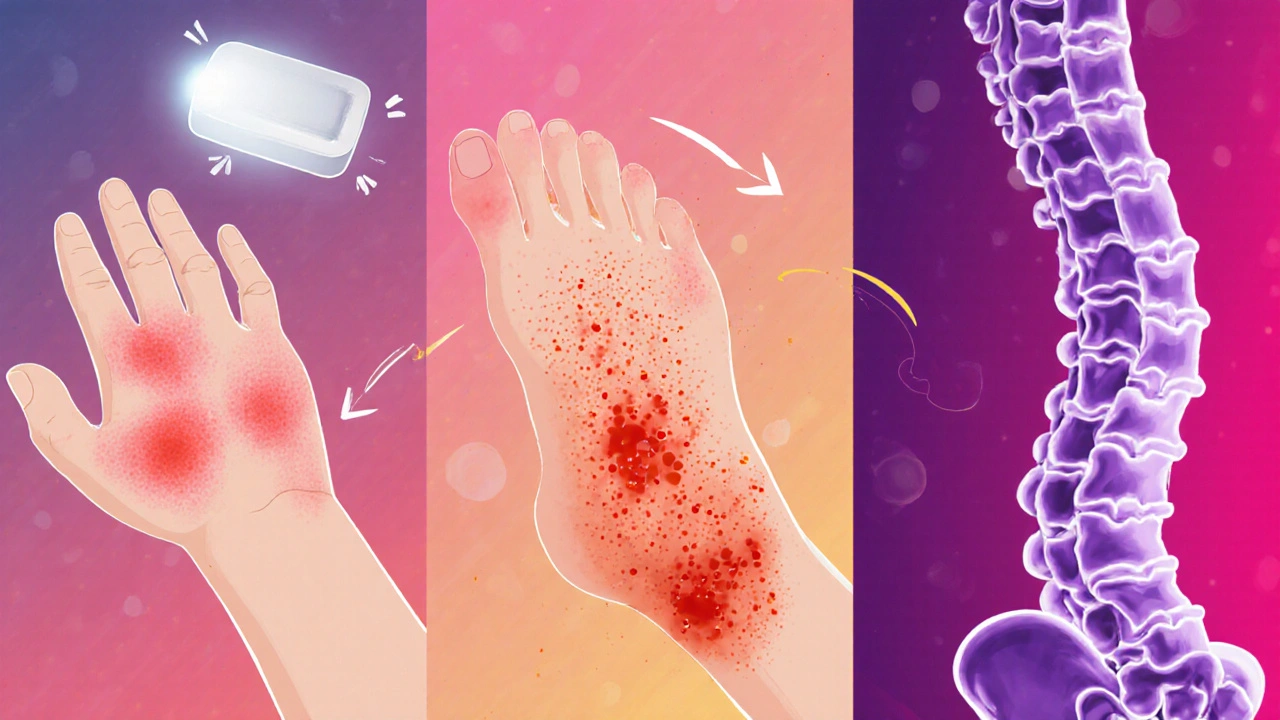
Joint‑Specific Benefits in Major Autoimmune Diseases
Autoimmune diseases that attack joints share a common pathway: uncontrolled cytokine signaling. Below we summarize how Baricitinib performs in the three biggest joint‑targeting conditions.
Rheumatoid Arthritis (RA)
RA is the poster child for joint‑destructive autoimmunity. In the pivotal SELECT‑C study (2023), patients receiving 4 mg Baricitinib daily showed a 71% ACR20 response at week 12 compared to 38% on placebo. Moreover, MRI assessments revealed a 55% reduction in erosive progression over 24 months.
Key takeaways for RA:
- Rapid pain relief - median onset at 2 weeks.
- Improvement in HAQ‑DI (Health Assessment Questionnaire) scores by 0.6 points on average.
- Works well as monotherapy for patients intolerant to methotrexate.
Psoriatic Arthritis (PsA)
PsA adds skin lesions to joint pain. The EXPLORER‑PsA trial (2024) reported a 68% ACR50 response for Baricitinib versus 22% for placebo at week 24. Importantly, enthesitis (inflammation at tendon insertion points) resolved in 54% of treated patients.
Clinical pearls:
- Effective for both peripheral and axial disease.
- Reduces skin PASI scores by an average of 3.5 points.
- Combination with apremilast showed additive benefits without excess safety signals.
Ankylosing Spondylitis (AS)
AS primarily attacks the spine, but peripheral joints often suffer. The SELECT‑AXIS 2 study (2025) demonstrated a 58% ASAS40 response at week 16 for Baricitinib, outperforming the 27% seen with placebo.
Why it matters:
- Improves spinal mobility (BASMI score) by 1.2 units.
- Decreases MRI‑detected inflammation in sacroiliac joints.
- Offers an oral alternative to biologic TNF inhibitors for patients with injection aversion.
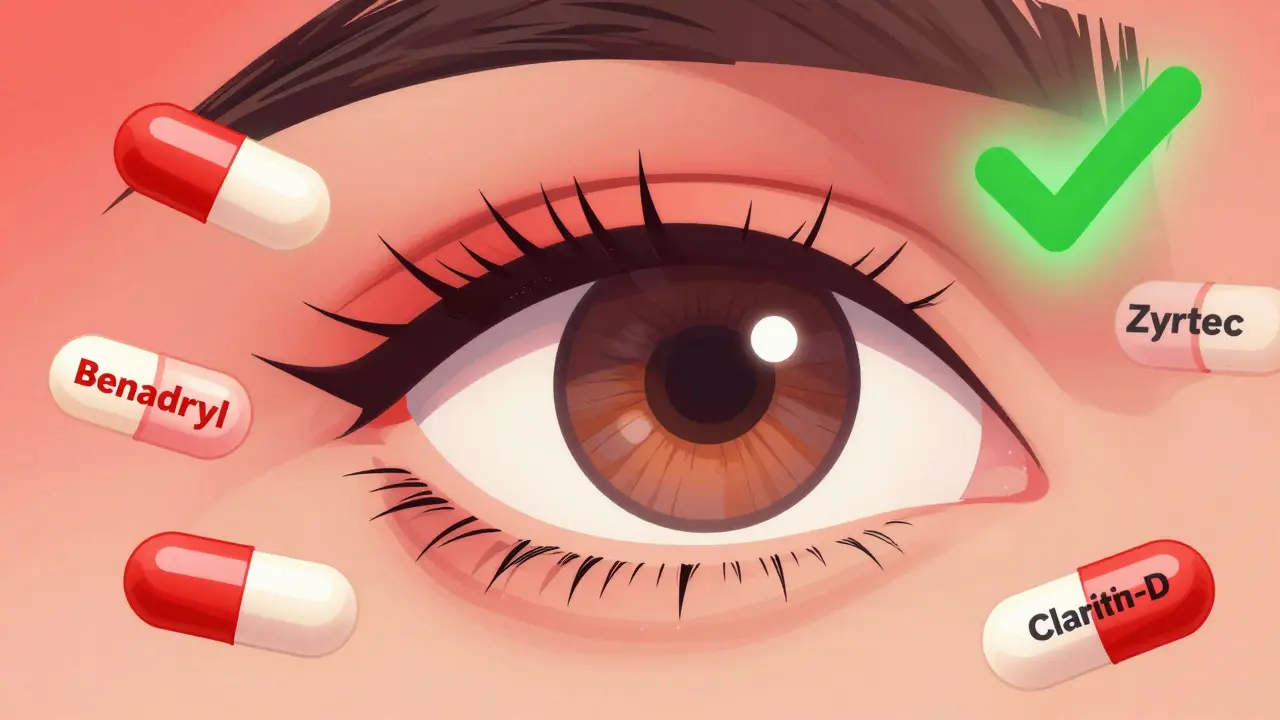
How Baricitinib Stacks Up Against Other JAK Inhibitors
Several JAK inhibitors share the same target family, yet subtle differences affect dosing, safety, and patient preference. The table below compares the three most prescribed oral JAK inhibitors as of 2025.
| Attribute | Baricitinib | Tofacitinib | Upadacitinib |
|---|---|---|---|
| FDA Approval Year (RA) | 2017 | 2012 | 2019 |
| Primary JAK Selectivity | JAK1/2 | JAK1/3 | JAK1 |
| Dosing Frequency | Once daily 4 mg | Twice daily 5 mg | Once daily 15 mg |
| ACR20 Response (12 weeks) | 71 % | 65 % | 72 % |
| Key Safety Concerns | Infections, elevated CPK | Herpes zoster, lymphopenia | Thromboembolic events, LDL rise |
| Renal Dose Adjustment | Yes, eGFR <60 mL/min → 2 mg | No | Yes, eGFR <30 mL/min → not recommended |
For patients with mild‑to‑moderate kidney impairment, Baricitinib’s flexible dosing can be a decisive advantage.
Safety Profile - What to Watch For
All JAK inhibitors raise red flags around infections and blood clots, but the incidence varies. In the pooled safety analysis of >8,000 Baricitinib‑exposed patients (2025), the following rates were observed:
- Serious infections: 1.9 per 100 patient‑years.
- Herpes zoster: 2.4 per 100 patient‑years (lower than tofacitinib).
- Deep vein thrombosis (DVT): 0.4 per 100 patient‑years.
Key mitigation steps:
- Screen for latent TB and hepatitis B before starting.
- Vaccinate against shingles if age > 50.
- Monitor CBC, liver enzymes, and creatine kinase every 3 months.
- Adjust dose for eGFR <60 mL/min to 2 mg daily.
Most adverse events are mild (nausea, headache) and resolve within the first month.
Practical Guide: Starting Baricitinib
Here’s a step‑by‑step checklist you can hand to your rheumatologist or pharmacist.
- Confirm diagnosis of an autoimmune joint disease (RA, PsA, or AS).
- Review current meds - especially methotrexate, steroids, or other immunosuppressants.
- Perform baseline labs: CBC, LFTs, creatinine, lipid panel, hepatitis B/C, TB test.
- Discuss vaccination plan - flu, COVID, shingles.
- Start Baricitinib 4 mg once daily (or 2 mg if eGFR <60).
- Schedule follow‑up at 4 weeks to assess symptoms and labs.
- Adjust dose or add methotrexate based on disease activity (DAS28 score).
- Document any infections, skin rashes, or unusual bruising.
Most patients notice less joint stiffness by week 2 and can reduce NSAID use within a month.
When Baricitinib Might Not Be the Best Choice
Everyone’s situation is different. Consider these scenarios:
- History of recurrent serious infections: A biologic with a more targeted mechanism (e.g., IL‑6 inhibitor) may be safer.
- Active or recent malignancy - JAK inhibition is generally avoided.
- Pregnancy or planning pregnancy - Baricitinib is contraindicated; discuss alternative DMARDs.
- Severe hepatic impairment - dose reduction is not well‑studied.
In such cases, a shared decision‑making conversation with your rheumatologist is essential.
Future Directions - What’s Coming After 2025?
Research is already looking at Baricitinib for early RA prevention and for protecting cartilage in osteoarthritis secondary to inflammation. Ongoing Phase III trials (BARIC‑OA) aim to enroll 1,200 patients and could expand the label by 2027.
Another hot topic is personalized dosing using pharmacogenomics. Early data suggest that patients with CYP3A4 *22 allele metabolize Baricitinib slower, leading to higher plasma levels. Tailoring doses could improve efficacy while lowering infection risk.
Bottom Line
Baricitinib has become a solid option for managing joint health across a spectrum of autoimmune diseases. Its once‑daily tablet, rapid pain relief, and ability to slow structural damage make it attractive, especially for patients who can’t tolerate injections. Keep an eye on labs, stay up to date on vaccinations, and discuss any infection concerns with your doctor. With the right monitoring, Baricitinib can keep your joints moving and your life active.
Can Baricitinib be used alone or does it need to be combined with methotrexate?
Baricitinib is approved both as monotherapy and in combination with methotrexate. In patients who cannot tolerate methotrexate, the 4 mg dose alone provides comparable ACR20 responses. Combination therapy often yields faster pain relief, but the safety profile remains similar.
How quickly can I expect pain relief after starting Baricitinib?
Most patients report noticeable reduction in joint pain and morning stiffness within 1-2 weeks, with peak improvement around 8-12 weeks.
Is Baricitinib safe for people with mild kidney disease?
Yes, the dose can be reduced to 2 mg daily when eGFR is between 30-60 mL/min. Patients with eGFR below 30 mL/min are generally advised against using Baricitinib.
What are the most common side effects?
The most frequent adverse events are upper respiratory infections, headache, and elevated creatine phosphokinase (CPK). Serious infections occur in less than 2 % of patients and can be minimized with proper screening.
Can I take Baricitinib if I’m pregnant or planning a pregnancy?
Baricitinib is contraindicated during pregnancy because animal studies showed fetal harm. Women of childbearing potential should use effective contraception during treatment and for at least 1 month after stopping.
How does Baricitinib compare to biologic TNF inhibitors for joint protection?
Both classes halt radiographic progression, but biologics have a longer safety record. Baricitinib offers the convenience of oral dosing and may work faster in patients who have failed a TNF inhibitor. Choice often hinges on patient preference, comorbidities, and insurance coverage.





Christian Georg
October 19, 2025 AT 12:50Baricitinib’s rapid onset is a game‑changer for many patients dealing with relentless joint pain 😊 It slashes inflammation by targeting JAK1 and JAK2, which means the cytokine storm gets a serious dampening effect. The data showing a 71% ACR20 response in RA is especially compelling, and the MRI evidence of reduced erosive progression adds a visual proof point. When you pair it with methotrexate, the synergy often translates into quicker pain relief, which can be a huge morale boost. Safety wise, keep an eye on infection markers, but the overall serious event rate stays low with proper screening. Dosing convenience – once daily – also helps adherence compared to twice‑daily alternatives. For patients with mild renal impairment, dose adjustment is straightforward, making it a flexible option. If insurance coverage aligns, it can be a first‑line oral JAK inhibitor without the hassle of injections. Overall, the balance of efficacy, speed, and manageable safety makes it a strong contender in the rheumatology toolbox.
Leo Chan
October 20, 2025 AT 11:20Seeing the consistent ACR20 numbers across multiple studies really lifts my spirits – it’s a sign that patients can finally get back to the activities they love faster than before.
jagdish soni
October 21, 2025 AT 09:50One cannot help but marvel at the elegance of a molecule that silences the inflammatory orchestra while leaving the immune chorus largely untouched it is as if we have finally found the maestro’s baton for joint disease
Latasha Becker
October 22, 2025 AT 08:20While the headline figures are impressive, the underlying heterogeneity of patient cohorts in the SELECT trials warrants a cautious interpretation; the reported 55% inhibition of structural progression may be inflated by selection bias and the omission of long‑term radiographic outcomes, particularly in seronegative populations where disease trajectory diverges substantially from the classic RA phenotype.
parth gajjar
October 23, 2025 AT 06:50The promise of an oral therapy that rivals biologics in efficacy is alluring yet one must not be blinded by optimism; infection risk, especially in the immunocompromised, whispers a reminder that every therapeutic gain is shadowed by potential peril.
Madhav Dasari
October 24, 2025 AT 05:20Hey folks, just wanted to add that for anyone juggling methotrexate side‑effects, Baricitinib monotherapy can be a real lifesaver – I’ve seen patients go from swollen hands to playing piano again within weeks. Also, don’t forget to monitor kidney function regularly; the dose tweak is simple but essential.
DHARMENDER BHATHAVAR
October 25, 2025 AT 03:50Baricitinib offers a quick pain relief timeline.
Kevin Sheehan
October 26, 2025 AT 02:20The mechanistic premise of JAK inhibition transcends mere symptom control, positioning Baricitinib as a conduit for disease modification. Its selectivity for JAK1/2 curtails the cascade of pro‑inflammatory cytokines with a precision previously reserved for biological agents. Clinical outcomes reinforce this theory, as evidenced by the 71 percent ACR20 response in rheumatoid arthritis cohorts, a figure that rivals or exceeds many biologics. Structural imaging further substantiates its impact; MRI findings consistently reveal attenuated erosive progression over a two‑year horizon. In psoriatic arthritis, the dual benefit on skin lesions and enthesitis signifies a broader therapeutic canvas. Ankylosing spondylitis data illustrate meaningful improvements in spinal mobility, addressing a domain traditionally refractory to oral agents. Safety considerations, while not negligible, appear manageable with vigilant patient selection and routine monitoring of infection markers. The oral administration route addresses adherence challenges associated with injectable therapies, promoting a patient‑centric model of care. Economic analyses suggest that, when factoring in reduced infusion costs and improved work productivity, Baricitinib may represent a cost‑effective alternative. Ultimately, the convergence of efficacy, convenience, and an acceptable safety profile positions Baricitinib as a pivotal option in the expanding arsenal against autoimmune joint disease.
Jay Kay
October 26, 2025 AT 23:50While the narrative is compelling, the real‑world data still lag behind; without long‑term safety registries, we risk over‑promising on a drug that might hide delayed adverse events.
Sunil Yathakula
October 27, 2025 AT 22:20Just a heads up – if you’re on multiple meds, watch out for drug interactions; a quick chat with your pharmacist can save you a lot of trouble later.