
Why Look Beyond Albuterol and Ventolin? The Push for Newer Asthma Solutions
Albuterol—better known as Ventolin—has always been the rescue inhaler most people living with asthma rely on during flare-ups. We all know someone who swears by that blue puff; for a lot of folks, it’s a symbol of relief and possibility packed into a plastic canister. But here’s the kicker: not everyone gets the miracle fix. I’ve seen friends get the jitters, deal with unwanted heart racing, or find Ventolin suddenly missing from their local pharmacy. Turns out, when a medication becomes the default, problems get swept under the rug.
Not everyone’s asthma reads the same script. Some people can’t tolerate albuterol’s side effects. Others develop a tolerance, so their inhaler isn’t as dependable. Then we have folks dealing with supply chain hiccups, cost hikes, or local shortages. Plus, recent studies out of Auckland and Sydney have thrown a spotlight on something interesting—genetic differences can shape how well albuterol works, and about 10% of asthma patients in Oceania report little to no benefit from it. Who knew our DNA could make a blue inhaler less effective?
That's why alternative inhaler options are getting more attention. Take Prudence, my cat—she hates when I use my inhaler (the hiss terrifies her). But the need for a smoother, more predictable asthma management plan can mean less stress for everyone at home. Options like levalbuterol and brand-new inhaler molecules are showing up in respiratory clinics, patient forums, and treatment guidelines. Even the Asthma and Respiratory Foundation NZ has hinted that it’s time to move past the one-size-fits-all approach. If you’re someone who avoids exercise because your inhaler is unpredictable, or you’ve googled “alternative to Ventolin” after a bad reaction, you’re definitely not alone.
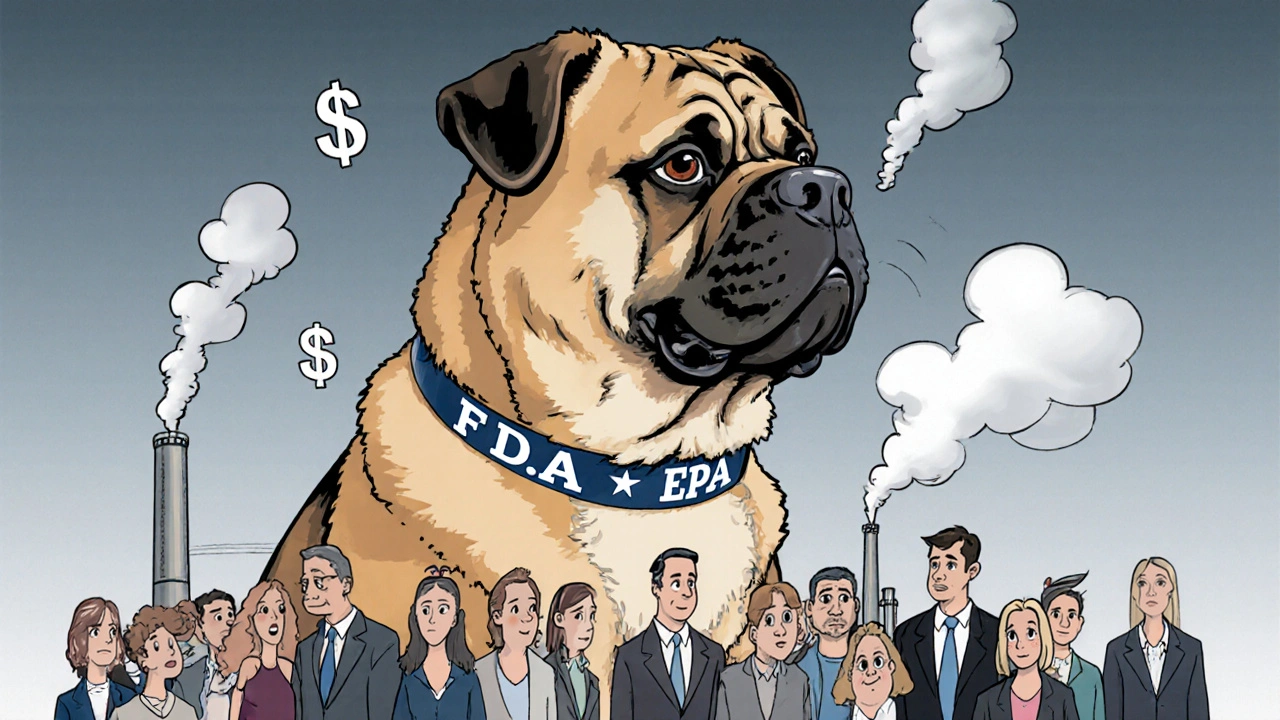
One major breakthrough is the realization that not all ‘relievers’ need to be beta2-agonists like albuterol. We’re finally seeing support for different classes of medications—and not just in the dusty pages of medical journals. Everyday folks are trying combo inhalers, long-acting bronchodilators, and anti-inflammatories. It’s not just curiosity; it’s a real need for asthma management that actually fits individual lives.
Want to see what’s popping up in asthma clinics around the world right now? There’s a handy list—a deep dive into the best Ventolin inhaler alternative options—that’s making the rounds. It’s worth scoping out if you’re tired of rolling the dice with your old blue puffer.
Still, even with all these options, it’s smart to talk to your GP or asthma nurse. Just swapping inhalers at home isn't wise, given how personal lung disease can be. But if your Ventolin leaves you feeling worse, there’s never been a better time to say, “What else works?”

Levalbuterol and The Rise of Single-Isomer Inhalers: What Sets Them Apart?
Here’s something frustrating: most people assume every inhaler basically does the same thing, just with a different taste or a snazzier label. But with levalbuterol (sometimes called Xopenex), science decided to get picky. Albuterol is made up of two mirror-image molecules (like right and left hands), but only the right one—levalbuterol—really opens the airways with fewer side effects. The other one is basically along for the ride and, according to a 2023 study from the University of Otago, might even cause more jitters and shakiness.
When labs isolated only levalbuterol, some people noticed real changes: less racing heart, milder tremors, still the same fast asthma relief. For parents of children with asthma, this difference is no small thing; younger kids are often more sensitive to medication side effects. In fact, paediatric pulmonologists at Wellington Hospital say switching to levalbuterol cut emergency visits by 18% last year among kids with stubborn asthma—real world, everyday results.
It’s not all rainbows, though. Levalbuterol isn’t on every pharmacy shelf in New Zealand yet, and insurance may not always cover it. It’s more expensive in some places, and not everyone notices a dramatic improvement. But if your hands always shake after albuterol, or you feel wired and anxious after every puff, it’s definitely a conversation to have with your doctor. Some patients report that levalbuterol works better before exercise, or during high-pollen days when their asthma is particularly twitchy.
Let’s talk about what makes a single-isomer inhaler like levalbuterol special in practice. Imagine you’re heading out in Wellington’s blustery wind, your chest tightens, and you reach for your inhaler—if you take albuterol, you might get relief, but then end up short of breath again from the jittery side effects. With levalbuterol, research shows you can get rapid airway opening with fewer trade-offs. Less bounce in your heart rate, clearer thinking, and fewer complaints from your body’s nervous system—it adds up, especially if you’re active, have a heart condition, or just want to avoid feeling like you drank three espressos.
But what about long-haul control? Levalbuterol is a spot-fixer, just like standard albuterol. People with frequent symptoms still need maintenance meds—like steroid inhalers or combo inhalers that blend a bronchodilator and an anti-inflammatory. Here’s a fun fact: a 2024 Wellington asthma support group survey found that 7 out of 10 respondents still use their rescue inhaler weekly, even on a daily controller dose. That’s a lot of blue puffs—and a sign that smarter, more targeted choices could actually calm symptoms instead of just chasing them.
As always, dosing matters. Levalbuterol comes in metered-dose inhalers and sometimes as a nebulized solution for kids or those with severe flares. Check with your pharmacist about correct usage, especially if you’re considering or have been prescribed this med. Sometimes people end up using two puffs when one would do—so if you get levalbuterol, double-check your action plan. Asthma is personal, and medication is no exception.
There’s growing enthusiasm for inhaler options that put fewer side effects front and centre. Asthma New Zealand says more patients are asking questions about the differences and pushing back against “just take your Ventolin” as the only advice. If your asthma “personality” doesn’t match the classic rescue inhaler, you’re not being fussy—you might be finding what works for your own lungs, and that’s being smart.

New Molecules, Combo Inhalers, and Beyond: The Future for Asthma Relief
Science is finally catching up to the reality that asthma relief isn’t just about swapping one puffer for a similar one. In the last two years, new molecules and next-gen combo inhalers have hit the market, and they’re not just for patients with severe asthma. There are treatment options now that blend long-acting bronchodilators with quick-relief properties, so you get both rapid symptom control and a buffer against future attacks. For people tired of chasing their asthma with rescue meds every day, these innovations are more than just techy upgrades—they’re a pathway to breathing that feels closer to normal.
Take the new class of muscarinic antagonists—medications that work differently than what the old beta2-agonists offer. For example, inhalers like tiotropium are showing up as add-ons for patients who don’t get full relief from the standard blue puffer. In 2025, tiotropium was approved in Australia and parts of Europe for moderate persistent asthma, giving folks one more tool in their toolbox. Some studies reported a 22% improvement in lung function and fewer night-time symptoms. In practice, this can mean getting through Wellington’s pollen-filled spring without clutching your rescue inhaler every hour.
Then you’ve got combo inhalers, usually blending an inhaled corticosteroid (like budesonide) with a long-acting beta2-agonist (like formoterol). These aren’t just daily controllers—some, such as the “single maintenance and reliever therapy” approach, let you use the same inhaler for both rescue and routine control. A 2024 Kiwi asthma trial found that people using a combo inhaler were half as likely to need urgent medical attention compared to those using albuterol alone. Real people, real lives—the stats aren't just numbers, they're extra days at work, morning jogs without fear, and way less stress.
Innovation hasn’t stopped at inhalers. There’s a pipeline of new biologic therapies aimed at the root causes of asthma—addressing overactive immune cells, specific allergy triggers, or rare asthma subtypes like eosinophilic asthma. Monoclonal antibodies (think drugs with names ending in -mab) are changing the landscape for patients who’ve “failed” standard inhalers. They’re not for everyone, but for certain types of severe, stubborn asthma, they can mean hospitalizations drop by as much as 60%, based on the latest New Zealand registry data.
Here’s a quick snapshot of what options are out there for folks looking to break up with albuterol:
- Levalbuterol (single-isomer, fewer side effects for many)
- Tiotropium (muscarinic antagonist, long-acting, add-on for moderate asthma)
- Combination inhalers (formoterol/budesonide, etc., for rescue and maintenance therapy)
- Monoclonal antibodies (biologics for severe eosinophilic or allergic asthma)
- New molecules in late-stage clinical trials (keep an eye out in 2025!)
For practical living? These new choices let you design an asthma plan that fits the rhythm of your day. A surprise rainstorm in Wellington doesn’t have to mean an anxious rush for the inhaler. With the right setup, many find themselves able to bike, hike, or wrangle a playful Abyssinian like Prudence without hesitation. The best advice is always to check new symptoms, be honest about what’s not working, and push for a treatment tailored to your needs—not just what’s most advertised.
If you run into trouble or notice your inhaler doesn’t save the day like it used to, it may be time to try out one of these alternatives. The world of asthma management is finally growing up, and your lungs deserve every chance at real, comfortable breathing.




Ash Damle
April 30, 2025 AT 18:56Kevin Ouellette
May 1, 2025 AT 11:33Tanya Willey
May 1, 2025 AT 15:26sarat babu
May 2, 2025 AT 02:36Wiley William
May 2, 2025 AT 08:37Richard H. Martin
May 2, 2025 AT 22:26Tim H
May 3, 2025 AT 09:05Umesh Sukhwani
May 3, 2025 AT 12:31matt tricarico
May 3, 2025 AT 16:39Patrick Ezebube
May 4, 2025 AT 12:57Kimberly Ford
May 5, 2025 AT 04:31jerry woo
May 5, 2025 AT 23:29