Understanding Secondary Hyperparathyroidism
Before we delve into the connection between secondary hyperparathyroidism and gastrointestinal issues, it's important to first understand what secondary hyperparathyroidism is. This condition is characterized by an excessive production of parathyroid hormone (PTH) by the parathyroid glands in response to low levels of calcium in the blood. Secondary hyperparathyroidism is often caused by conditions that affect the body's ability to maintain calcium levels, such as kidney disease or vitamin D deficiency.
This condition can lead to a range of symptoms, including bone pain, fatigue, muscle weakness, and depression. However, research also suggests a link between secondary hyperparathyroidism and gastrointestinal issues, which we will explore further in this article.
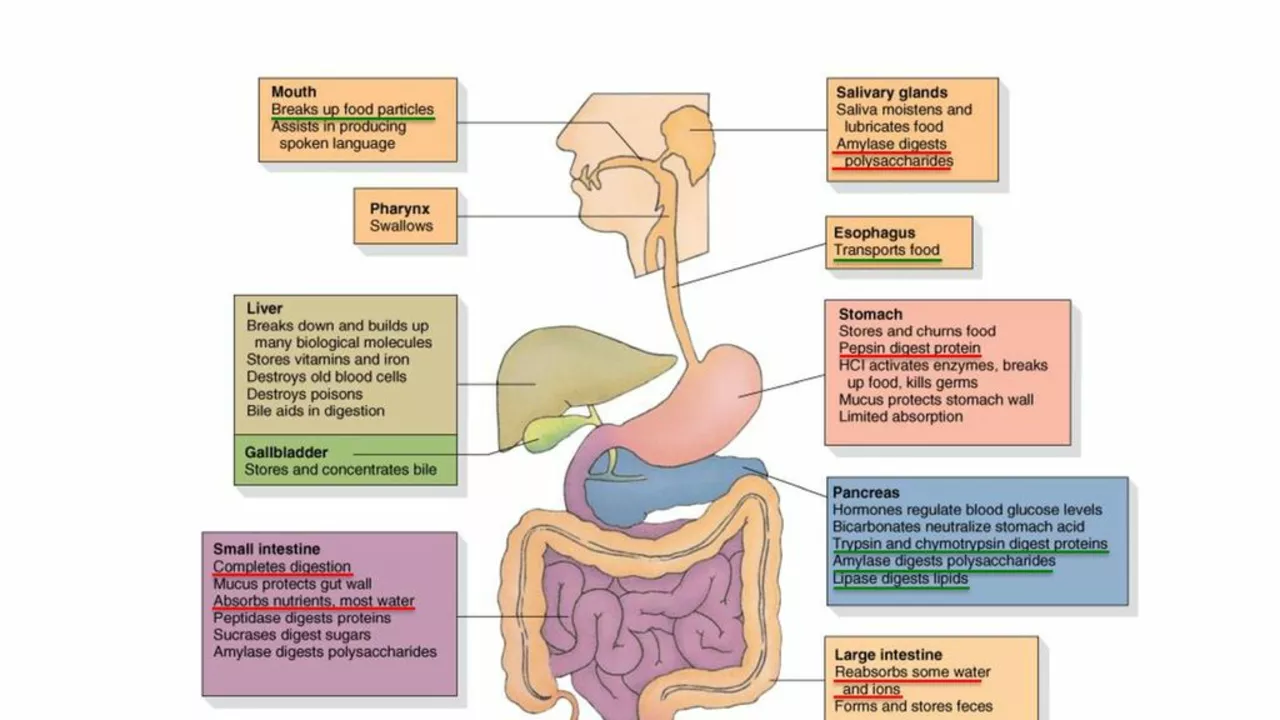
The Role of Parathyroid Hormone in Digestive Health
Parathyroid hormone plays a crucial role in maintaining the body's calcium balance. Yet, its functions are not limited to bone health. PTH also influences the digestive system. This hormone stimulates the production of gastric acid in the stomach, a crucial component for digestion. Therefore, an overproduction of PTH can potentially lead to an overproduction of gastric acid, causing a range of gastrointestinal issues such as heartburn, indigestion, and gastritis.
Secondary Hyperparathyroidism and Gastroesophageal Reflux Disease
One of the most common gastrointestinal issues associated with secondary hyperparathyroidism is gastroesophageal reflux disease (GERD). GERD is a chronic condition characterized by the backflow of stomach acid into the esophagus, which can cause heartburn and damage to the esophagus. The excessive gastric acid production stimulated by high levels of PTH can contribute to the development of GERD, making this a common complication in individuals with secondary hyperparathyroidism.
Peptic Ulcers and Secondary Hyperparathyroidism
Another gastrointestinal condition that can be linked to secondary hyperparathyroidism is peptic ulcers. These are sores that develop on the lining of the stomach, upper small intestine or esophagus, often as a result of excessive gastric acid. Given that secondary hyperparathyroidism can stimulate the overproduction of gastric acid, individuals with this condition may be at an increased risk of developing peptic ulcers.
Secondary Hyperparathyroidism and Malabsorption
Secondary hyperparathyroidism can also influence the absorption of nutrients in the gut. The excess PTH can alter the pH levels in the stomach, affecting the activation of certain enzymes necessary for digestion. This could potentially lead to malabsorption, where the body is unable to fully absorb nutrients from the food we eat, leading to deficiencies and associated health issues.
Impact of Vitamin D Deficiency
As mentioned earlier, vitamin D deficiency is a common cause of secondary hyperparathyroidism. Vitamin D plays a crucial role in calcium absorption in the gut. A deficiency in this vitamin can therefore lead to low calcium levels, triggering secondary hyperparathyroidism. Moreover, vitamin D deficiency itself can contribute to gastrointestinal issues, such as inflammatory bowel disease and colorectal cancer, thus compounding the potential for digestive problems in individuals with secondary hyperparathyroidism.
Treatment and Management
Management of secondary hyperparathyroidism primarily involves treating the underlying cause, such as kidney disease or vitamin D deficiency. In some cases, medication or surgery may be necessary to reduce PTH production. It's also crucial to manage any associated gastrointestinal issues. This can involve lifestyle modifications, such as dietary changes or stress management, as well as medication to control symptoms.
Conclusion
While secondary hyperparathyroidism is primarily associated with bone health, it's clear that this condition can also have significant impacts on the digestive system. Understanding these connections is crucial for effective management and treatment. As always, if you're experiencing symptoms of secondary hyperparathyroidism or gastrointestinal issues, be sure to consult with a healthcare professional.




jerry woo
July 2, 2023 AT 12:51Jillian Fisher
July 3, 2023 AT 04:10Rachel Marco-Havens
July 3, 2023 AT 17:03Kathryn Conant
July 4, 2023 AT 00:21j jon
July 4, 2023 AT 15:02Jules Tompkins
July 5, 2023 AT 03:02Sabrina Bergas
July 5, 2023 AT 11:00Melvin Thoede
July 6, 2023 AT 01:19Suzanne Lucas
July 6, 2023 AT 14:41Ash Damle
July 6, 2023 AT 15:33Kevin Ouellette
July 7, 2023 AT 00:16Tanya Willey
July 7, 2023 AT 20:59matt tricarico
July 8, 2023 AT 07:17sarat babu
July 9, 2023 AT 01:53