Glaucoma Medication Risk Checker
Check Your Medications
Enter medications you're currently taking. Include allergy, cold, sleep aids, or any over-the-counter drugs.
Key Safety Information
Avoid immediately
Medications containing diphenhydramine, chlorpheniramine, pseudoephedrine, or phenylephrine may cause sudden vision loss in narrow-angle glaucoma. Stop taking these immediately if you experience eye pain or blurred vision.
Risk Assessment
Enter medications to see your risk assessment
Type medication names separated by commas
Most people reach for antihistamines when their eyes water, their nose runs, or their throat itches. But if you have glaucoma - especially a specific type called narrow-angle glaucoma - those same pills could trigger a medical emergency. You might not even know you’re at risk. That’s the scary part.
What’s the Real Danger?
Not all glaucoma is the same. About 70% of people with glaucoma have primary open-angle glaucoma (POAG). For them, most over-the-counter allergy meds are fine. But the other 10-15% have narrow-angle glaucoma. That’s where things get dangerous.Narrow-angle glaucoma means the space between your iris and cornea is too tight. Normally, fluid drains out of your eye through that angle. But when antihistamines like diphenhydramine (Benadryl) or chlorpheniramine cause your pupils to dilate, they can physically block that drainage channel. Fluid builds up. Pressure spikes. In hours, you could lose vision - permanently.
This isn’t theoretical. A study in the PMC database found that people taking daily doses of certain antidepressants had over a fivefold increase in acute angle-closure glaucoma. Antihistamines do the same thing. They’re not just drying your nose - they’re tightening the screws inside your eye.
Which Medications Are Risky?
It’s not just allergy pills. Many cold, flu, and sleep aids contain the same ingredients. Here’s what to watch for:- Diphenhydramine - found in Benadryl, Tylenol PM, Advil PM
- Chlorpheniramine - common in cold and allergy combos
- Pseudoephedrine and phenylephrine - decongestants in Sudafed, Claritin-D, Zyrtec-D
- Meclizine and Phenergan - anti-nausea meds
- Steroid nasal sprays or eye drops - even short-term use can raise pressure
- Topiramate (Topamax) - used for migraines and seizures
- Sulfa-based drugs - like sulfamethoxazole
These aren’t rare drugs. They’re on nearly every pharmacy shelf. And they’re often sold without clear warnings about glaucoma. Many people don’t realize they’re taking something that could blind them.
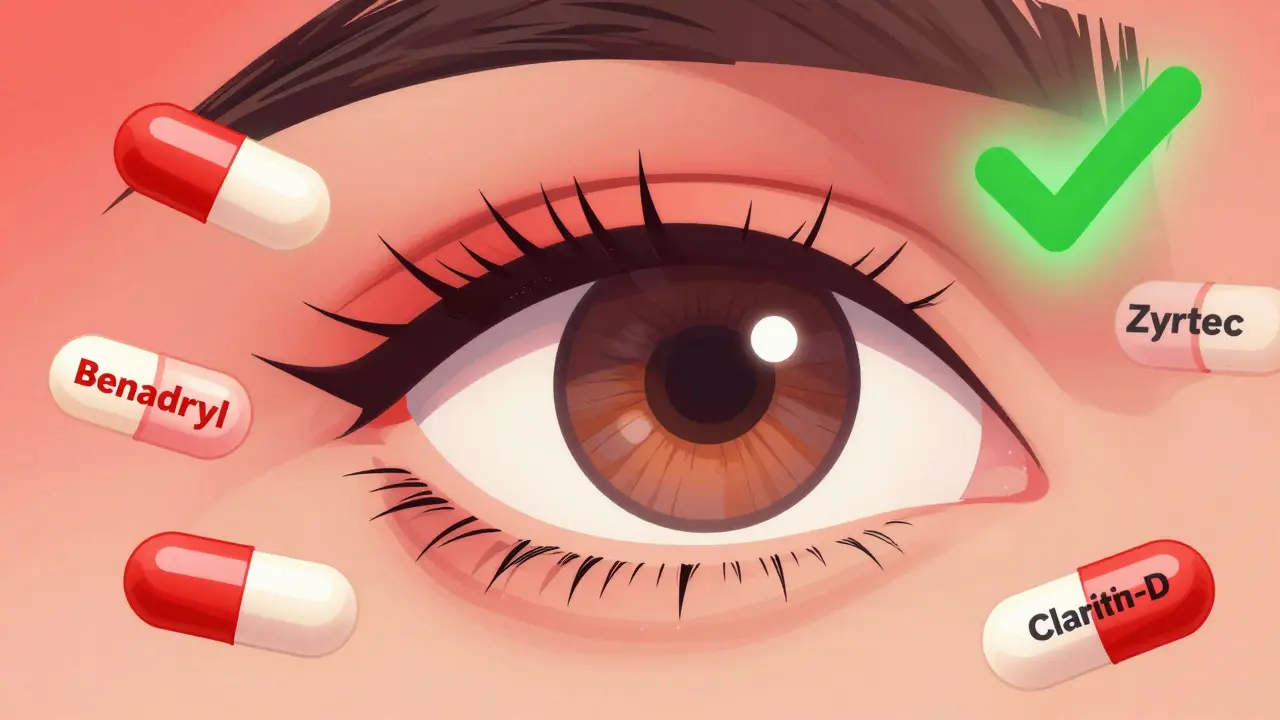
What About Second-Generation Antihistamines?
Good news: not all antihistamines are created equal. Second-generation ones like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) have much lower anticholinergic activity. They don’t cross into the eye as easily. That means they’re generally safer for people with glaucoma - even narrow-angle.But “generally safer” doesn’t mean “safe for everyone.” Your eye anatomy matters more than the drug label. Some people with very tight angles still react. Always check with your eye doctor before switching or starting any new medication, even if it’s labeled “non-drowsy” or “allergy-specific.”
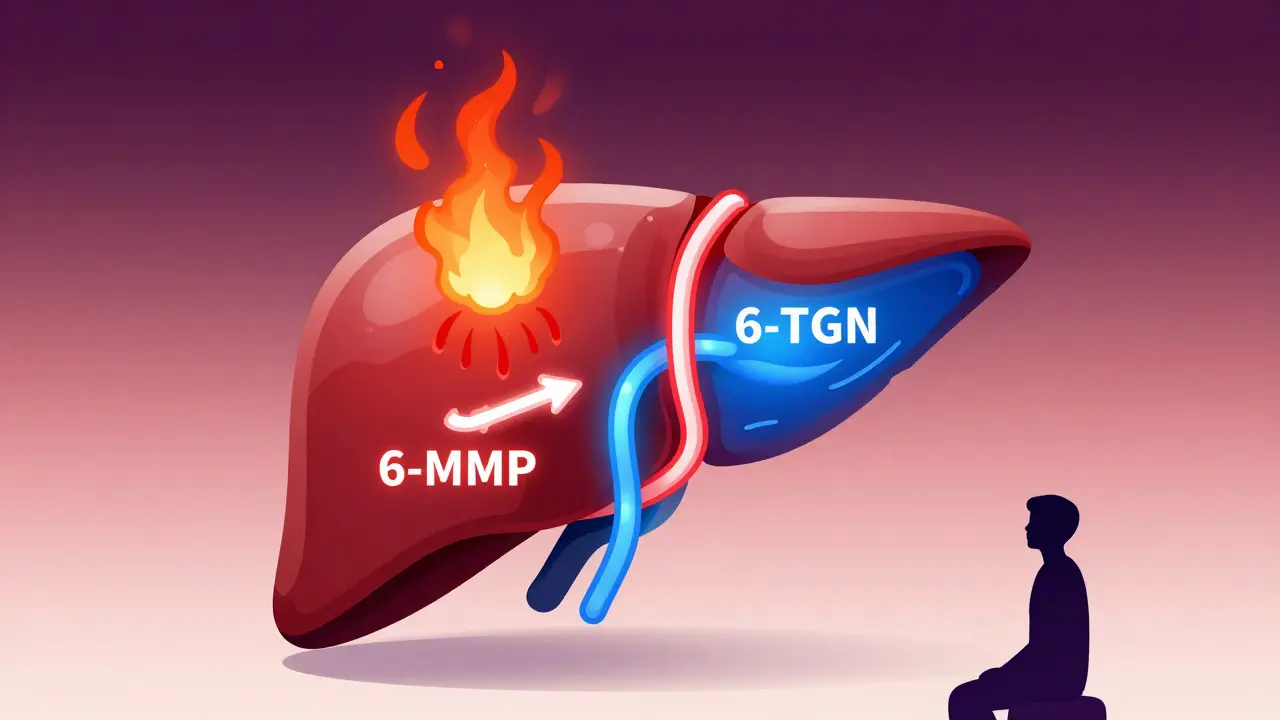
Steroids Are a Hidden Threat
Steroid nasal sprays, eye drops, and even oral steroids can raise eye pressure over time. This doesn’t cause sudden angle closure. Instead, it slowly leads to open-angle glaucoma - the kind you don’t feel until it’s advanced.How? The theory is that steroids cause proteins to build up in the eye’s drainage system, like gunk clogging a sink. After ten days of regular use, the risk jumps. That’s why your eye doctor will want to check your pressure if you’ve been using a steroid spray for more than a week.

What If You’ve Already Had Surgery?
Some people with narrow-angle glaucoma have had a laser procedure called a peripheral iridotomy. This creates a tiny hole in the iris to let fluid flow freely. It’s highly effective. Many patients who’ve had this can use antihistamines without issue.But even then - don’t assume. Surgery reduces risk, not eliminates it. Other factors like age, other medications, or new eye changes can still matter. Always tell your eye doctor what you’re taking, even if you think you’re “safe.”
Who’s Most at Risk?
You’re more likely to have narrow-angle glaucoma if you’re:- Over 40
- Female
- Of Asian or Inuit descent
- Farsighted (hyperopic)
- Have a family history of glaucoma
Many people don’t know they have it until they take a medication and suddenly get:
- Severe eye pain
- Blurred vision
- Halos around lights
- Nausea or vomiting
- Sudden loss of vision
This is an emergency. Call your eye doctor or go to the ER. Waiting even an hour can mean the difference between saving your sight and losing it.
What Should You Do?
If you have glaucoma - or think you might - here’s what to do right now:- Find out your exact type. Ask your eye doctor: “Do I have open-angle or narrow-angle glaucoma?” If they don’t know, get a second opinion. Gonioscopy - a simple, painless test - can confirm this in minutes.
- Check every medication label. Look for diphenhydramine, chlorpheniramine, pseudoephedrine, or phenylephrine. If you see them, don’t take them unless your eye doctor says it’s okay.
- Use safer alternatives. Stick with loratadine, cetirizine, or fexofenadine. These are your best bet for allergy relief without the risk.
- Limit steroid sprays. Don’t use them longer than 10 days without checking your eye pressure.
- Carry medical info. Keep a card in your wallet or use a phone app that says: “I have narrow-angle glaucoma. Avoid anticholinergics.” Emergency staff won’t know your history - you have to tell them.

Why Isn’t This Better Warned?
It’s frustrating - and dangerous - that OTC meds don’t clearly warn about glaucoma. The FDA doesn’t require it. Most packaging says “consult your doctor if you have heart disease or high blood pressure,” but nothing about your eyes.Glaucoma UK reports that their helpline gets dozens of calls every month from people who accidentally triggered an attack after taking Benadryl or a cold tablet. Many didn’t even know they had glaucoma. Others knew they had “glaucoma” but didn’t know the type.
Advocacy groups are pushing for change. But until labels improve, you have to be your own advocate.
What About Natural Alternatives?
You’ll find online claims about “natural antihistamines” like quercetin, stinging nettle, or vitamin C. Some people swear by them. But there’s no solid evidence they work as well as prescription or OTC meds - especially for severe allergies.And here’s the catch: even if they help, they’re not regulated. You don’t know the dose, purity, or interactions. For someone with narrow-angle glaucoma, guessing isn’t worth the risk. Stick with proven, doctor-approved options.
Is There Hope for the Future?
Yes. Research is moving in the right direction. A 2023 clinical trial is testing a new version of loratadine designed to stay out of the eye. Other studies show statins - drugs for cholesterol - might actually help slow open-angle glaucoma progression. That’s promising.But the biggest breakthrough isn’t a new drug. It’s awareness. More eye doctors are now doing gonioscopy on everyone over 40 during routine exams. That’s how you catch narrow angles before they cause trouble.
If you’ve never had this test, ask for it. It takes less than five minutes. It could save your vision.
Can I take Benadryl if I have glaucoma?
No - if you have narrow-angle glaucoma, Benadryl (diphenhydramine) can trigger a sudden, sight-threatening spike in eye pressure. Even if you think you have "regular" glaucoma, never assume. Always confirm your type with your eye doctor before taking any antihistamine.
Are Zyrtec and Claritin safe for glaucoma?
Yes - loratadine (Claritin) and cetirizine (Zyrtec) are second-generation antihistamines with minimal effect on the eye’s drainage system. They’re generally considered safe for most glaucoma patients, including those with narrow angles. Still, always confirm with your eye doctor before starting any new medication.
Can steroid nasal sprays cause glaucoma?
Yes - long-term or repeated use of steroid nasal sprays, eye drops, or pills can raise intraocular pressure and lead to open-angle glaucoma. This usually happens after 10 or more days of use. If you’ve been using them for over a week, ask your eye doctor to check your pressure.
What should I do if I suddenly have eye pain and blurred vision?
This could be acute angle-closure glaucoma - a medical emergency. Stop taking any allergy or cold meds immediately. Go to the nearest emergency room or call your eye doctor right away. Delaying treatment can cause permanent vision loss within hours.
Do I need a special test to know if I have narrow-angle glaucoma?
Yes - a routine eye exam won’t always catch it. You need gonioscopy, a simple, painless test where the doctor uses a special lens to view the drainage angle in your eye. If you’re over 40 or have a family history of glaucoma, ask for this test during your next visit.




Kunal Majumder
January 10, 2026 AT 15:16Man, I had no idea Benadryl could do this to your eyes. My grandma takes it every night for sleep and she’s got glaucoma. Gonna talk to her doctor tomorrow. Thanks for laying this out so clear.
Aurora Memo
January 12, 2026 AT 10:02This is one of those posts that should be mandatory reading before you buy anything at the pharmacy. I’m glad someone took the time to explain the difference between open-angle and narrow-angle. So many people assume ‘glaucoma’ is one thing.
Ian Cheung
January 12, 2026 AT 19:05Look I get it antihistamines are everywhere but seriously why does the FDA let this slide? It’s like they’re playing Russian roulette with people’s vision. I took Claritin-D last winter and my eyes felt weird but I just blamed it on dry air. Now I’m sweating bullets thinking I almost blinded myself. This is wild.
Also shoutout to the guy who mentioned gonioscopy - that test is the unsung hero of eye health. My doc did it on me at 42 and saved my sight. No drama no pain just a little flash of light and boom you know if you’re ticking time bomb.
And yeah Zyrtec and Allegra are your new BFFs. Skip the PM stuff. Even if you’re tired just go to bed early. Your eyes will thank you more than that extra hour of sleep ever could.
Also steroid sprays? Yeah I used Flonase for three months straight after a bad cold. My pressure went up like a balloon. Doc caught it. I’m alive. Don’t be me.
Christine Milne
January 13, 2026 AT 11:38It is regrettable that the American public has become so lethargic in its medical literacy. The onus for safety does not rest upon pharmaceutical manufacturers, but upon the individual who chooses to ingest substances without first consulting a licensed ophthalmologist. The proliferation of over-the-counter medications is not a failure of regulation, but of personal responsibility. One cannot blame the FDA for the populace’s refusal to read labels or seek professional guidance.
Bradford Beardall
January 15, 2026 AT 08:40Just curious - in India, do doctors routinely screen for narrow-angle glaucoma? I’ve heard in some places it’s not part of standard exams unless you’re symptomatic. Would love to hear from someone who’s had that test done there.
McCarthy Halverson
January 16, 2026 AT 01:20Check your meds. Check your eyes. Don’t wait till it’s too late.
Ashlee Montgomery
January 16, 2026 AT 21:18I wonder how many people have lost vision because they thought ‘it’s just an allergy pill’ - and how many doctors assume patients already know the risks. The system fails when education is left to chance. This isn’t just about drugs. It’s about who gets access to the information that could save them.
neeraj maor
January 17, 2026 AT 18:37Let’s be real - this whole thing is a pharmaceutical distraction. They don’t want you to know that natural remedies work better. Quercetin, vitamin C, even local honey - they’ve been suppressing this for decades. The ‘danger’ of antihistamines? A smokescreen. They make billions off your fear. Your eye doctor? Probably on their payroll. Gonioscopy? Just a money grab. Trust your body, not the lab coats.
Ritwik Bose
January 19, 2026 AT 17:10Thank you for sharing this vital information. I have narrow-angle glaucoma and was unaware that even steroid nasal sprays posed a risk. I will immediately consult my ophthalmologist regarding my current medication regimen. 🙏