
When you’re facing cancer that can be removed with surgery, the timing of treatment matters just as much as the treatment itself. Should you start chemotherapy or immunotherapy before the operation to shrink the tumor? Or wait until after surgery to kill off any leftover cancer cells? This isn’t just a medical debate-it’s a real decision that affects how you feel, how long you wait for surgery, and even your chances of survival.
What Neoadjuvant Therapy Actually Does
Neoadjuvant therapy means giving treatment-usually chemo, immunotherapy, or both-before surgery. It’s not about replacing surgery. It’s about making surgery more effective. Think of it like clearing a path before building a house. If the tumor is too big or too close to vital structures, surgery might be risky or impossible. Neoadjuvant therapy shrinks it first.
In non-small cell lung cancer (NSCLC), the CheckMate 816 trial showed that combining nivolumab (an immunotherapy) with chemo before surgery led to a 24% pathologic complete response rate. That means in nearly one in four patients, no living cancer cells were found in the removed tumor. Compare that to just 2.2% with chemo alone. That’s not just a statistic-it’s hope. Patients who achieve this level of response live longer.
For triple-negative breast cancer, neoadjuvant chemo is now standard for many patients. Around 30-40% achieve a pathologic complete response, and those patients have a much better long-term outlook. The big advantage? You find out right away if the drugs are working. If the tumor shrinks dramatically, you know the treatment is hitting the right targets. If it doesn’t? Doctors can adjust what comes next-maybe switching drugs or planning more aggressive follow-up.
Why Adjuvant Therapy Still Has a Place
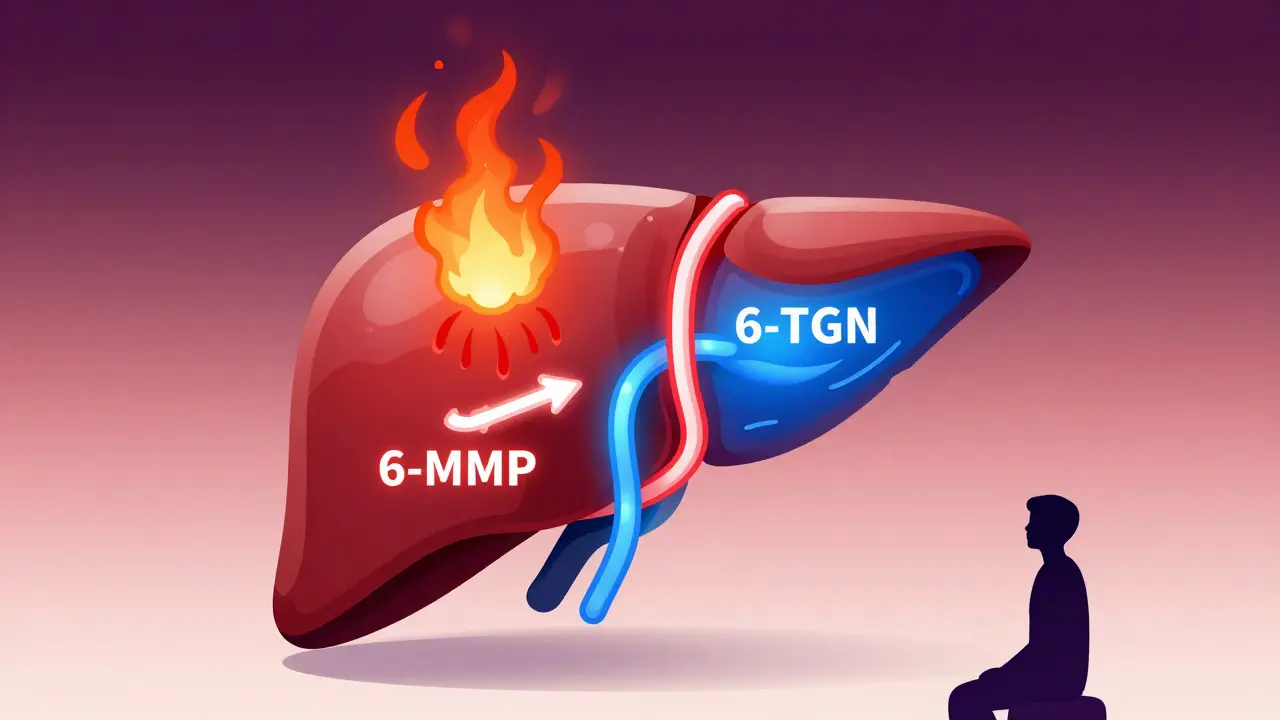
Adjuvant therapy happens after surgery. The idea is simple: even if the surgeon removes every visible tumor, tiny cancer cells might still be hiding elsewhere in the body. Adjuvant treatment wipes those out before they grow into new tumors.
This approach has been the backbone of cancer care for decades. In breast cancer, adjuvant chemo has been shown to reduce recurrence by up to 30% in high-risk cases. For colon cancer, it cuts the chance of the cancer coming back by half. It’s proven. Reliable. Predictable.
But here’s the catch: you’re giving powerful drugs to someone who’s already been through surgery. Recovery is hard. Fatigue sets in. Nausea hits. And you’re treating based on guesswork-you don’t know for sure if the cancer responded to the drugs until months later, if it comes back.
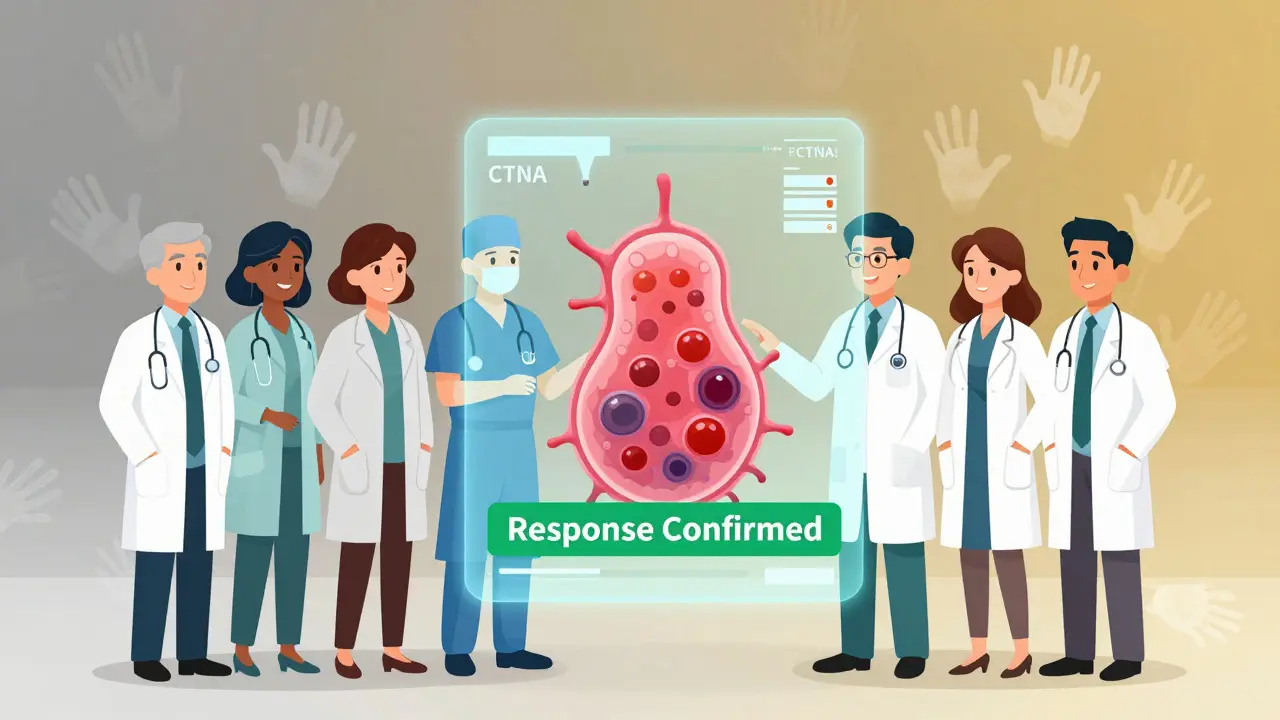
The Real Difference: Seeing the Response
The biggest shift in cancer care over the last five years isn’t new drugs-it’s the ability to see how the tumor reacts in real time. Neoadjuvant therapy turns treatment into a live test. You give the drugs. You wait. You scan. You see if the cancer dies. Then you operate.
In NSCLC, this has changed everything. The American Society of Clinical Oncology now says neoadjuvant chemoimmunotherapy is preferred for stage IB to IIIA disease. Why? Because if a patient gets a pathologic complete response, they don’t need as much follow-up treatment. Some don’t need adjuvant therapy at all.
A 2024 meta-analysis of over 3,200 patients found that adding adjuvant immunotherapy after neoadjuvant therapy didn’t improve survival-but it did increase serious side effects. Nearly 30% of patients on the combo had grade 3 or higher side effects like lung inflammation, liver damage, or severe fatigue. That’s almost double the rate of those who stopped after neoadjuvant treatment.
That’s why top oncologists like Dr. Mark Awad at Dana-Farber are saying: if you get a strong response upfront, you might not need more. Save the toxicity for when it’s truly needed.
Who Gets Which Approach?
Not everyone is a candidate for neoadjuvant therapy. It’s not a one-size-fits-all. The decision depends on cancer type, stage, and biology.
- Non-small cell lung cancer (NSCLC): If your tumor is stage IB (over 4 cm) to IIIA and you’re healthy enough for surgery, neoadjuvant chemoimmunotherapy is now the standard. PD-L1 expression levels help decide if immunotherapy will help.
- Triple-negative breast cancer: Neoadjuvant chemo is recommended for stage II or III. If you get a complete response, your survival odds jump significantly.
- HER2-positive breast cancer: Neoadjuvant therapy with targeted drugs like trastuzumab and pertuzumab is common. Pathologic response predicts long-term outcomes.
- Hormone receptor-positive breast cancer: Often treated with surgery first, then hormone therapy. Neoadjuvant chemo is used if the tumor is large or aggressive.
- Rectal cancer: Neoadjuvant chemoradiation is standard before surgery to shrink tumors and lower recurrence risk.
For some cancers, like early-stage prostate or thyroid cancer, surgery alone is enough. Neoadjuvant or adjuvant therapy isn’t needed.
The Timing Matters-More Than You Think
It’s not just about what you give, but when you give it. After neoadjuvant therapy ends, surgery should happen within 3 to 6 weeks. Too soon, and your body hasn’t recovered from the drugs. Too late, and the tumor might start growing again.
Adjuvant therapy usually starts within 6 to 8 weeks after surgery, once healing is complete. Delaying it beyond 12 weeks reduces its effectiveness.
Coordination is key. You need surgeons, oncologists, radiologists, and pathologists all talking. But here’s the problem: only 58% of community hospitals have formal neoadjuvant pathways. In academic centers, it’s 92%. If you’re not near a major cancer center, you might have to fight for the right approach.
What Patients Are Saying
On patient forums, stories reveal the emotional weight of these choices.
One NSCLC patient said: “My oncologist said, ‘Let’s see if the drugs kill the cancer before we cut.’ We got lucky-I had over 90% tumor kill. That gave me peace of mind.”
Another breast cancer patient shared: “I chose adjuvant chemo because I wanted surgery done. Later, I found out I had triple-negative cancer. I wish I’d known that neoadjuvant could have told me if the chemo would work.”
A 2023 survey found that 62% of NSCLC patients on neoadjuvant therapy felt anxious during the waiting period. They feared the cancer would spread while they waited for surgery. That’s real stress. But 78% of oncologists now offer neoadjuvant immunotherapy for early-stage lung cancer-up from 42% just three years ago.
The Future Is Personalized
What’s coming next? Blood tests. Not just any blood tests-liquid biopsies that detect circulating tumor DNA (ctDNA). After neoadjuvant therapy, if ctDNA is still present in the blood, it means cancer cells are hiding. Those patients get adjuvant therapy. If ctDNA is gone? They might skip it.
Trials like KEYNOTE-867 and NeoADAURA are testing this exact idea. In the next five years, doctors won’t just decide based on tumor size or stage. They’ll decide based on what the cancer’s DNA tells them.
The goal? To give the right treatment, to the right patient, at the right time-and avoid giving too much to those who don’t need it.
What You Need to Ask Your Doctor
If you’re facing surgery for cancer, these are the questions that matter:
- Is neoadjuvant therapy an option for my cancer type and stage?
- What’s the chance I’ll get a pathologic complete response?
- Will we test for PD-L1 or other biomarkers before starting?
- What are the risks of delaying surgery?
- Will you check for ctDNA after treatment to guide next steps?
- Do you recommend stopping immunotherapy after surgery, or continuing?
There’s no perfect answer. But the trend is clear: more doctors are choosing neoadjuvant therapy first-not because it’s newer, but because it gives more information. And in cancer care, information is power.
Market Shifts and What They Mean
The global market for neoadjuvant therapy is growing fast-projected to hit $29.3 billion by 2028. Why? Because more patients are getting it. In the U.S., 35% of stage II-III NSCLC patients now get neoadjuvant chemoimmunotherapy, up from 15% in 2020. In breast cancer, it’s jumped from 8% in 2005 to 35% today.
Regulatory agencies have caught up. The FDA approved neoadjuvant nivolumab for NSCLC in 2022. The EMA did the same. Insurance companies are following. This isn’t experimental anymore. It’s standard.
But access still varies. If you’re in a rural area or a smaller hospital, you might need to ask for a referral to a center that does this regularly. Don’t be afraid to push. Your survival depends on getting the right sequencing-not just the right drugs.





Chris Urdilas
January 28, 2026 AT 23:32So let me get this straight-we’re giving people chemo and immunotherapy BEFORE cutting them open, just so we can see if the drugs work? And if they do, we skip the after-party treatment? That’s not medicine, that’s like ordering a pizza and only paying if the pepperoni’s fresh.
But honestly? I’m here for it. If I’m gonna get blasted with drugs, I want proof they’re doing something before they slice me open. No more guessing games. My uncle got adjuvant chemo after surgery and still came back with metastases. I’d rather know upfront if the drugs are trash or treasure.
Jeffrey Carroll
January 30, 2026 AT 18:33The shift toward neoadjuvant therapy represents a significant evolution in oncologic care, grounded in robust clinical evidence and biomarker-driven decision-making. The pathologic complete response rate observed in CheckMate 816 is not merely statistically significant-it is clinically transformative.
Moreover, the reduction in unnecessary adjuvant therapy following a strong neoadjuvant response mitigates systemic toxicity, aligning with the ethical imperative of minimizing harm while maximizing therapeutic benefit. The integration of liquid biopsy for ctDNA monitoring further refines this paradigm, heralding a truly personalized approach to cancer management.
Phil Davis
February 1, 2026 AT 03:41Wow. So now we’re all supposed to be excited because doctors are finally doing something that makes sense? Took them long enough.
I mean, sure, you could’ve just told me the tumor’s dead before you cut it out. Instead, we spent 20 years cutting people open, then poisoning them afterward like it was a ritual. Classic medicine: fix it, then blame the patient if it comes back.
Now we’re doing science? Cool. Let’s just make sure it’s not just another $$$-driven trend disguised as progress.
Irebami Soyinka
February 3, 2026 AT 00:14USA be thinking they invented medicine now? 😒
We in Nigeria, we still fight for basic chemo-no fancy immunotherapy, no ctDNA tests, no ‘neoadjuvant pathways.’ You talk about ‘standard of care’ like it’s a luxury yacht. Meanwhile, my cousin’s mom waited 6 months just to get a biopsy.
But hey, if you got the cash and the clinic, go ahead and shrink that tumor before cutting. We’ll celebrate when every African woman with breast cancer gets the same shot.
✊ #CancerIsNotACountryClub
Kevin Kennett
February 4, 2026 AT 08:47Look, I get why this is a big deal. But let’s not pretend this is some magic bullet. Neoadjuvant therapy sounds awesome until you’re the one sitting in that waiting room for six weeks, scared the tumor’s gonna grow while you wait for surgery. I’ve seen patients break down over scans.
And don’t even get me started on access. My buddy in rural Ohio got told, ‘We don’t do that here.’ So he drove 3 hours every week for chemo, then flew to Chicago for surgery. That’s not healthcare-that’s a survival marathon.
We need to fix the system before we celebrate the science. Real talk.
Jess Bevis
February 5, 2026 AT 01:14ctDNA is the future. If it’s gone, you’re done. Simple.
Rose Palmer
February 6, 2026 AT 15:56The clinical data supporting neoadjuvant chemoimmunotherapy in non-small cell lung cancer is unequivocal and has been formally endorsed by both the American Society of Clinical Oncology and regulatory bodies such as the FDA and EMA. The reduction in pathologic tumor burden correlates directly with improved disease-free and overall survival.
Furthermore, the elimination of adjuvant therapy in patients achieving pathologic complete response represents a paradigmatic shift toward de-escalation of treatment intensity, thereby minimizing iatrogenic harm while preserving therapeutic efficacy. This is precision oncology in practice.
However, equitable access remains a critical challenge. Institutional infrastructure, multidisciplinary coordination, and patient education must be prioritized to ensure that these advances are not confined to academic centers.
Kathy Scaman
February 7, 2026 AT 14:09My aunt did neoadjuvant for her breast cancer. She got the full response. No chemo after. She’s been cancer-free for 4 years now.
She says the waiting was hell. But the relief? Worth every second.
Also, the docs didn’t even mention ctDNA until she asked. So yeah-ask questions. Don’t just nod.