
Many people don’t realize that drinking alcohol while taking medication can be as risky as taking the wrong pill. It’s not just about getting drunk faster - it’s about your body reacting in ways that can land you in the emergency room, or worse. The truth is, alcohol and medications don’t mix safely in most cases. Even if you’re only having one drink, the combination can turn a routine treatment into a life-threatening situation.
How Alcohol Changes How Medications Work
Alcohol doesn’t just sit there quietly. It actively interferes with how your body processes medicines. Two main things happen: your liver gets overwhelmed, and your brain gets extra depressed. Your liver is responsible for breaking down both alcohol and most medications. When you drink, your liver prioritizes alcohol because it’s a toxin. That means your meds sit around longer, building up in your system. For some drugs, that means stronger effects. For others, it means they don’t work at all. At the same time, alcohol slows down your central nervous system. So do many medications - like sleep aids, painkillers, and anxiety drugs. When you combine them, the effect isn’t just added - it’s multiplied. That’s why mixing alcohol with opioids or benzodiazepines can shut down your breathing. The FDA has documented cases where people died after drinking just a few drinks while taking these meds.Deadly Combinations You Need to Avoid
Some drug-alcohol pairings are so dangerous they’re listed in black box warnings - the strongest warning the FDA can give. Opioids like oxycodone, hydrocodone, and methadone become far more dangerous with alcohol. In 2020, 20% of opioid overdose deaths involved alcohol. Extended-release versions are especially risky. Alcohol can cause the pill to release all its drug at once, flooding your system. That’s what led to the removal of Palladone in 2005. Benzodiazepines like Xanax, Valium, and Ativan are another major concern. Mixing them with alcohol increases your risk of overdose by 24 times, according to a 2019 study. These drugs already cause drowsiness and poor coordination. Add alcohol, and you’re looking at a high chance of falling, choking, or stopping breathing. Acetaminophen (Tylenol) is one of the most common over-the-counter painkillers. But when combined with alcohol, it becomes a silent liver killer. The liver turns acetaminophen into a toxic chemical called NAPQI. Normally, your body neutralizes it with glutathione. But alcohol depletes glutathione. Without it, NAPQI builds up and destroys liver cells. The FDA says this combination causes about 56,000 ER visits and 458 deaths every year in the U.S. alone. Metronidazole (Flagyl), an antibiotic used for infections, triggers a violent reaction with alcohol. It causes nausea, vomiting, flushing, rapid heartbeat, and chest pain - even with just one drink. You need to wait at least 72 hours after your last dose before drinking.Other High-Risk Medications
Not all dangerous combinations are obvious. Some are sneaky. NSAIDs like ibuprofen (Advil) and naproxen (Aleve) already irritate your stomach lining. Alcohol does the same. Together, they increase your risk of gastrointestinal bleeding by 3 to 5 times. That means internal bleeding you might not even notice until it’s too late. Antihistamines like Benadryl and Zyrtec are often taken for allergies or sleep. They make you drowsy. Alcohol makes you drowsier. The result? Poor balance, slow reactions, and a higher chance of falling - especially dangerous for older adults. ADHD meds like Adderall and Ritalin are stimulants. They mask how drunk you feel, so you might drink more than you realize. At the same time, they raise your heart rate and blood pressure. Alcohol lowers them. This tug-of-war puts stress on your heart and can lead to arrhythmias or sudden cardiac events. SSRIs like Prozac and Zoloft don’t cause dangerous physical reactions, but they don’t help either. Alcohol worsens depression and anxiety - the very symptoms these drugs are meant to treat. It also makes you more likely to skip doses or stop taking them altogether. Blood pressure medications can cause your blood pressure to drop too low when mixed with alcohol. This leads to dizziness, fainting, and falls. For older adults, a single fall can mean a broken hip and long-term disability.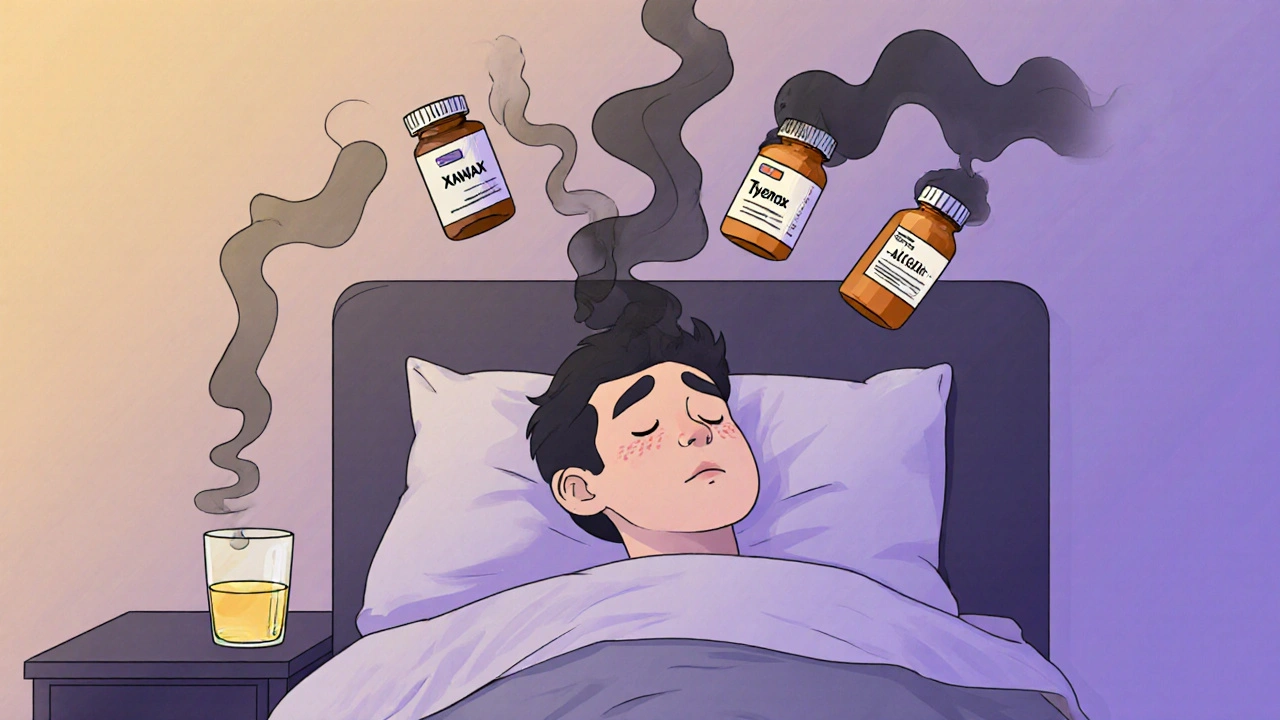
Who’s at Highest Risk?
Some people are far more vulnerable than others. People over 65 are at the top of the list. They take an average of 14 prescriptions a year. Their bodies process alcohol and drugs slower. Their liver and kidneys don’t work as well. They’re also more likely to be on multiple high-risk meds at once. The Beers Criteria, updated in 2019, lists 30 medications that are potentially dangerous for older adults when mixed with alcohol - including benzodiazepines, muscle relaxants, and first-gen antihistamines. Women are at higher risk too. Because of differences in body composition, women reach higher blood alcohol levels than men after drinking the same amount. That means even one drink can have a bigger impact on their meds. Veterans and people with mental health conditions are also at increased risk. The VA found that 30% of veteran suicides involved alcohol and prescription drugs. People with depression, anxiety, or PTSD are more likely to use both alcohol and medications, and they often don’t tell their doctors.What You Should Do
The good news? You can protect yourself.- Read the label. The FDA requires alcohol interaction warnings on about 100 prescription drugs and 700 over-the-counter products. Look for phrases like “Do not drink alcohol,” “May cause drowsiness,” or “Avoid alcohol.”
- Ask your pharmacist. They’re trained to spot dangerous combinations. When you pick up a new prescription, ask: “Can I drink alcohol with this?” Don’t assume it’s safe just because your doctor didn’t mention it.
- Keep a list. Write down every medication you take - including supplements and herbal remedies. Bring it to every doctor visit. Many interactions happen because no one has the full picture.
- Wait it out. If you’re on metronidazole, wait 72 hours after your last dose. For some medications, even 24 hours isn’t enough. When in doubt, skip the drink.
- Be honest with your doctor. If you drink, say so. About 70% of pharmacists report patients don’t tell them they drink. That means your doctor can’t warn you properly.

Special Cases: Diabetes and Liver Health
If you have diabetes, alcohol can be a minefield. Sulfonylureas like glipizide and glyburide can cause your blood sugar to crash dangerously low - up to 300% more likely if you drink. Even if you’re on metformin, alcohol raises your risk of lactic acidosis, a rare but deadly condition. The advice? Limit yourself to one drink per day, and never drink on an empty stomach. If you have liver disease - even mild fatty liver - alcohol can accelerate damage. Many medications are processed by the liver. When it’s already injured, those drugs stick around longer and cause more harm. Avoid alcohol completely if you have cirrhosis, hepatitis, or elevated liver enzymes.What’s Being Done to Stop This?
The medical world is waking up. In 2023, the American Medical Association made it a standard to screen all patients for alcohol use when prescribing high-risk meds. Electronic health records now have hard-stop alerts that block prescriptions if the patient has a history of alcohol use. The FDA now requires new extended-release opioids to be tested for alcohol interactions before approval. Research is also moving toward personalized medicine. Testing for the CYP2E1 gene variant can identify people who are 4.7 times more likely to suffer liver damage from acetaminophen and alcohol. The CDC launched its “Alcohol and Medicine Don’t Mix” campaign in January 2023 with $2.5 million in funding. Flyers in pharmacies, social media ads, and warning stickers on bottles are now common. But awareness is still low - only 35% of primary care doctors routinely ask about alcohol use during medication visits.Bottom Line
There’s no safe level of alcohol when you’re on most medications. Even one drink can be too much. The risks aren’t theoretical - they’re documented in emergency room data, FDA reports, and peer-reviewed studies. If you take any kind of prescription, over-the-counter, or herbal medication, assume alcohol is unsafe until proven otherwise. Don’t rely on memory. Don’t guess. Ask your pharmacist. Read the label. When in doubt, skip the drink. Your liver, your brain, and your life depend on it.Can I have one drink while taking painkillers?
It depends on the painkiller. For acetaminophen (Tylenol), even one drink increases liver damage risk. For opioids like oxycodone or hydrocodone, one drink can cause fatal breathing problems. For NSAIDs like ibuprofen, one drink raises your chance of stomach bleeding. If you’re on any pain medication, it’s safest to avoid alcohol completely.
What if I only drink on weekends?
If you’re taking daily medications - like blood pressure pills, antidepressants, or antibiotics - weekend drinking still puts you at risk. Your body doesn’t clear all the drugs by Monday. The interaction doesn’t care when you drink - it cares that alcohol and the drug are in your system at the same time.
Do herbal supplements interact with alcohol?
Yes. St. John’s Wort can increase drowsiness when mixed with alcohol. Kava, used for anxiety, can cause liver damage when combined with even small amounts of alcohol. Valerian root and melatonin both make you sleepier - and alcohol multiplies that effect. Always treat herbal supplements like real medicine - they can interact just as dangerously.
How long should I wait after stopping a medication before drinking?
It varies. For metronidazole, wait 72 hours. For some antidepressants or antipsychotics, wait 1-2 weeks. For extended-release opioids, the drug can stay in your system for days. Always ask your pharmacist for the specific timeline. Never assume it’s safe just because you feel fine.
Are there any medications that are safe with alcohol?
Some, like certain antihistamines (loratadine) or topical creams, have minimal interaction risk. But “minimal” doesn’t mean “safe.” Even low-risk combinations can become dangerous if you drink heavily, have liver problems, or take multiple meds. The safest rule is: if it’s not explicitly labeled as safe, assume it’s not.






Edward Hyde
December 1, 2025 AT 13:10Wow. So let me get this straight - if I want to have a goddamn beer after work while taking my Zoloft, I’m basically signing my own death warrant? Thanks for the cheerleading, doc. I’ll just keep drinking and pretending my therapist doesn’t know I’m a mess. At least the booze makes the meds feel less like a prison sentence.
And don’t even get me started on that ‘ask your pharmacist’ nonsense. You think they got time to explain this shit? They’re scanning your pills like a barcode while the next customer yells about their coupon not working.
Also, why is acetaminophen the villain here? It’s literally the only thing that takes the edge off my migraines. You want me to just scream into a pillow instead? Cool. Cool cool cool.
Charlotte Collins
December 1, 2025 AT 23:05The data here is accurate but presented with the emotional weight of a public service announcement from 1998. The real issue isn’t the chemical interactions - it’s the systemic failure to educate patients in accessible, non-patronizing ways. Pharmacies don’t hand out pamphlets. Doctors don’t ask. Insurance companies don’t fund outreach. And yet we act shocked when people die from a glass of wine and a pill.
The CDC campaign is a Band-Aid on a hemorrhage. We need mandatory pharmacist-led counseling for high-risk prescriptions. Not a sticker on the bottle. Not a checkbox in an EHR. Actual human interaction. But that costs money, and money talks louder than mortality statistics.
Also - why is there no mention of alcohol’s role in noncompliance? People stop taking their meds because they’re depressed. Then they drink to numb the depression. Then they die. It’s not the alcohol. It’s the untreated illness. And we treat the symptom, not the cause.
Margaret Stearns
December 3, 2025 AT 04:36Just wanted to say thank you for writing this. I’m 68 and on 11 meds. My doctor never told me about the alcohol thing. I thought one glass of wine was fine. Now I know better. I’ve stopped completely. My liver enzymes are down. I feel better. It’s not easy, but it’s worth it.
Also - I wrote down every pill I take on a card and keep it in my wallet. I showed it to my new pharmacist last week. He said he’d never seen anyone do that. He was impressed.
Small steps, right?
amit kuamr
December 4, 2025 AT 06:01India also have same problem but nobody care. People take antibiotics and drink beer like it is normal. Even doctors say one beer ok. Then they die. Why you write so long? Just say no alcohol with medicine. Simple. Why you need all this science? In village we say if medicine is strong then alcohol is poison. Done.
Also why you say women more at risk? In India women drink less. So problem less. Logic.
And herbal? Who care? Nobody use St Johns Wort here. Only cheap pills. So why talk about it?
Mary Ngo
December 5, 2025 AT 07:13Let’s be honest - this entire article is a distraction. The real danger isn’t alcohol and pills. It’s the pharmaceutical industry’s manipulation of public perception. Did you know that the FDA approved over 12,000 new drugs in the last decade - and less than 2% were tested for alcohol interactions? That’s not negligence. That’s intentional. They want you to believe it’s your fault for drinking, not theirs for not testing properly.
And why is there no mention of the opioid crisis being fueled by the very companies that now warn you about alcohol? Purdue Pharma knew. They knew. They buried the data. Now they’re selling you pamphlets like saints.
Also - the CDC campaign? Funded by the same companies that profit from prescription sales. Coincidence? I think not.
Wake up. This isn’t about health. It’s about control.
And yes - I’ve seen the EHR alerts. They’re designed to protect the hospital from lawsuits, not your life.
James Allen
December 6, 2025 AT 01:39As an American who served 8 years overseas, I’ve seen how other countries handle this. In Germany, they slap warning labels on every bottle in 12 languages. In Japan, pharmacists do face-to-face counseling. Here? We hand you a script and say ‘have a nice day.’
And yet we’re the ones who think we’re the healthiest nation on earth? Please. We’re the ones with the highest prescription rates, the highest overdose deaths, and the lowest doctor-patient trust.
Meanwhile, the VA is still ignoring veteran suicides linked to alcohol-med interactions because ‘it’s complicated.’ It’s not complicated. It’s criminal neglect.
And don’t get me started on how they treat women’s health. If a man drinks while on meds, he’s ‘a little wild.’ If a woman does it? She’s ‘unstable.’ Double standard. Always has been.
Kenny Leow
December 6, 2025 AT 18:41Just wanted to say - I’m from Singapore, and we have this thing called ‘Medicine Day’ where pharmacists host free community sessions. People bring their pill bottles. They get a checklist. They ask questions. No judgment. Just facts.
It’s simple. It works.
Also - I used to drink two beers with my blood pressure meds. Now I don’t. Not because I’m scared. Because I respect my body more. And honestly? I sleep better. My anxiety dropped. My wife noticed.
Small change. Big difference.
🍻 to not drinking - but also to being informed.
Stay safe, everyone.
Kelly Essenpreis
December 8, 2025 AT 17:21So let me get this straight - if I take ibuprofen and have a beer, I’m gonna bleed out internally? That’s it? That’s the whole point? You people act like alcohol is the devil and Tylenol is the angel. Newsflash - both are chemicals. Your body handles them. If you’re weak, that’s your problem.
Also - why is this even a thing? In the 70s, people drank whiskey with aspirin and lived to 90. Now we’re treating a glass of wine like a terrorist attack?
And why are you targeting older people? Like they’re too dumb to know what they’re doing? My grandma drank wine with her pills till she was 94. She didn’t die from it. She died from old age. Maybe we should stop scaring people and start trusting them.
Also - I’ve never heard of metronidazole. Probably because I’m not a drug addict.
Rachel Stanton
December 9, 2025 AT 06:12This is such an important conversation - and I want to expand on something the post mentions but doesn’t dive into: polypharmacy. Especially for older adults, taking 10+ meds means the risk isn’t just alcohol + one drug - it’s alcohol + drug A + drug B + drug C + herb X + supplement Y. The interactions become exponential, not additive.
Here’s what I tell my clients: create a ‘medication map.’ List every substance - including caffeine, CBD, and even grapefruit juice - and bring it to your pharmacist. They can run it through a drug interaction checker in seconds.
Also - if you’re on SSRIs and drinking, you’re not just worsening depression. You’re rewiring your brain’s reward system. Alcohol reduces serotonin long-term. SSRIs try to boost it. The tug-of-war creates emotional numbness. That’s not ‘just feeling blah’ - that’s neurochemical sabotage.
You’re not broken. You’re just outmatched by a system that doesn’t prioritize your safety. But you can still protect yourself. One step at a time.
Amber-Lynn Quinata
December 9, 2025 AT 16:23I’ve been sober for 3 years since my mom died from liver failure after mixing Tylenol and wine. She didn’t know. She thought ‘one glass’ was fine. She was 62. She had arthritis. She took 2 pills every 6 hours. She drank one glass with dinner. That’s all.
They didn’t even test her for alcohol in the ER. They assumed it was ‘natural causes.’
Now I see people posting ‘just one drink’ like it’s harmless. I want to scream. I want to cry. I want to hug them.
Please. Just don’t. Not even one. Not ever.
💔
Lauryn Smith
December 11, 2025 AT 00:42I’m a nurse and I see this every day. People are terrified to tell their doctors they drink. They think they’ll be judged. Or cut off meds. Or labeled an addict.
But here’s the truth - your doctor wants to help. They’re not your judge. They’re your partner.
I had a patient last week who was on metformin and drank 3 beers every Friday. He was scared to say anything. When he finally told me, we adjusted his meds, added a glucose monitor, and he’s now down to one beer - and his HbA1c dropped from 8.2 to 6.4.
Honesty saves lives. Not shame.
You’re not alone. And you’re not bad for drinking. You’re just human. Let’s work with that.
Bonnie Youn
December 12, 2025 AT 01:32YES YES YES. I’ve been screaming this from the rooftops for years. People think ‘I’m healthy, I’ll just have one’ - but your body doesn’t care about your intentions. It only cares about chemistry.
I used to take Ambien and have a glass of wine to ‘help me relax.’ One night I woke up at 3am in my driveway with my car keys in my hand. I had no memory of leaving the house. I called my doctor the next day. He said ‘you were lucky you didn’t die.’
Now I don’t drink. Period. I sleep better. I think clearer. My anxiety is gone.
You don’t need alcohol to unwind. You need rest. You need boundaries. You need to love yourself enough to say no.
And if you’re still reading this - you’re ready to change. Start today. One day at a time. You got this 💪❤️
Scotia Corley
December 13, 2025 AT 03:50While the article presents statistically valid data, it lacks contextual nuance regarding cultural and individual variability in alcohol metabolism. The assumption of universal risk is both scientifically reductive and ethically problematic. Genetic polymorphisms in ADH and ALDH enzymes result in over a 100-fold difference in ethanol clearance rates across populations. To apply a blanket prohibition without accounting for pharmacogenomics is not medicine - it is overregulation disguised as caution.
Furthermore, the conflation of recreational use with pathological dependence undermines patient autonomy. The physician’s role is not to dictate behavior, but to inform - and then respect the patient’s right to accept or decline risk.
This approach, while well-intentioned, risks creating a culture of fear rather than empowerment.
elizabeth muzichuk
December 14, 2025 AT 20:47They’re lying. They always lie. This whole ‘alcohol and meds don’t mix’ thing? It’s a cover-up. The real reason they don’t want you drinking is because they’re hiding the fact that most of these drugs are made from the same chemicals as alcohol. They’re just purified. Controlled. Patentable.
Alcohol is nature’s medicine. The pharmaceutical industry hates that. So they scare you into buying their expensive pills and then tell you not to drink with them. Classic. They want you dependent. They want you afraid. They want you paying monthly.
And don’t tell me about ‘liver damage.’ My grandpa drank whiskey every night and lived to 98. He never took a single pill. Coincidence? I think not.
Wake up. The system is rigged. Drink if you want. They can’t control you unless you let them.