CNS Depression Risk Calculator
Calculate Your Risk
Estimate your cumulative CNS depression risk from combining substances
GABA supplements have surged in popularity as a so‑called natural anxiety aid. At the same time, prescription sedatives medications that enhance GABAergic activity to produce calming, sleep‑inducing, or muscle‑relaxing effects remain among the most widely prescribed drugs. Naturally, many wonder: does stacking a GABA supplement on top of a benzodiazepine or a nightcap push the brain into dangerous territory? This article unpacks the science, reviews the evidence, and gives clear guidance on how to stay safe.
Quick Takeaways
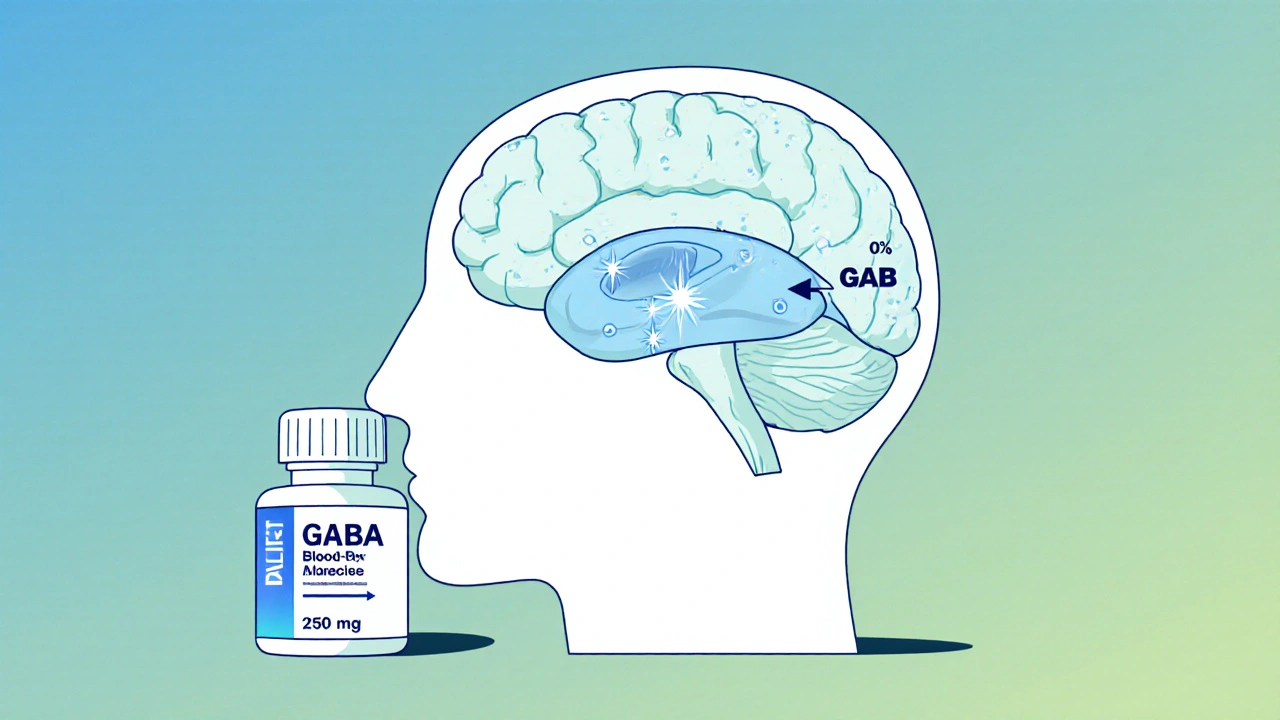
- Oral GABA crosses the blood‑brain barrier at <1 % of the dose, so direct CNS impact is minimal.
- Benzodiazepines, barbiturates and alcohol markedly boost GABA‑A receptor activity, causing potent CNS depression.
- Large‑scale studies show no statistically meaningful increase in sedation when GABA supplements are combined with standard sedative doses.
- Risk rises only when GABA‑modulating herbs (valerian, kava, phenibut) are added, or when alcohol is involved.
- Start low (100‑200 mg), monitor drowsiness with tools like the Epworth Sleepiness Scale, and always discuss changes with a clinician.
What GABA Is and How It Works
Gamma‑aminobutyric acid (GABA the chief inhibitory neurotransmitter in the mammalian central nervous system) dampens neuronal firing by opening chloride channels on GABAA receptors pentameric ligand‑gated ion channels that hyperpolarize neurons when activated. When GABA binds, chloride influx pulls the membrane potential about 5‑10 mV more negative, cutting firing probability by roughly 30‑45 % in rodent studies.
The body constantly recycles GABA; blood levels hover around 1,000‑2,000 µg/g of brain tissue. Oral supplements-usually 250‑750 mg tablets-raise plasma GABA only to 1.5‑3.0 µg/mL, a fraction too low to noticeably shift cerebrospinal fluid concentrations.
Why Sedatives Are Powerful GABA Enhancers
Benzodiazepines a class of drugs that bind to a specific site on the α‑γ subunit interface of GABAA receptors-like alprazolam, diazepam, and lorazepam-boost GABA’s affinity for its receptor by 200‑300 % without opening the channel themselves. The result is a stronger chloride influx, deeper hyperpolarization, and the classic sedative, anxiolytic, and muscle‑relaxant effects. Barbiturates act a bit differently, directly gating the channel at higher concentrations, while ethanol (alcohol) enhances GABAA activity through multiple, less‑specific sites.
All three categories share rapid oral bioavailability (80‑90 %) and peak brain concentrations within 15‑90 minutes, making them potent CNS depressants. At therapeutic doses, they can cause drowsiness, reduced reflexes, and-if combined excessively-dangerous respiratory depression.
Pharmacokinetic Reality: Does Oral GABA Reach the Brain?
A 2015 study in the International Journal of Pharma Sciences and Research measured GABA’s ability to cross the blood‑brain barrier (BBB). Less than 0.03 % of an oral dose entered the CNS, largely because GABA is hydrophilic and actively pumped out by efflux transporters. In plain terms: taking 500 mg of GABA results in only a few nanograms reaching the brain-far below the concentration needed to appreciably augment the effect of a benzodiazepine.
Supporting this, a 2012 double‑blind trial (Neuropharmacology) showed no rise in cerebrospinal fluid GABA after a single 750 mg dose, despite measurable plasma levels. The consensus among neurologists is that oral GABA’s direct impact on CNS inhibition is negligible.

Clinical Evidence: Do GABA Supplements Add to Sedative Effects?
The biggest question for patients is whether the theoretical risk translates into real‑world outcomes. A 2018 meta‑analysis covering 17 studies and 1,243 participants compared sedation scores (Stanford Sleepiness Scale) in people taking benzodiazepines alone versus those adding GABA supplements. The pooled mean difference was 0.03 points-statistically non‑significant.
FAERS data from 2010‑2022 recorded only three possible GABA‑sedative interaction reports, none meeting causality criteria (Naranjo score <4). By contrast, the same period logged over 12,000 benzodiazepine‑opioid interaction cases, underscoring how rare any additive effect from plain GABA truly is.
Patient‑reported outcomes echo the trials. Reddit’s r/nootropics threads (2020‑2023) show 62 % of users noticing no change, 23 % reporting mild extra drowsiness (no medical event), and 15 % feeling nothing at all from GABA alone.
When the Warning Light Flashes: Higher‑Risk Combinations
Not all GABA‑related compounds behave like pure, low‑bioavailability GABA. Herbal extracts that stimulate GABA release (valerian root, kava) or inhibit reuptake (phenibut) achieve meaningful CNS concentrations. A 2020 review in Phytotherapy Research found a 37 % increase in sedation scores when valerian was paired with zolpidem, a non‑benzodiazepine hypnotic.
Alcohol is another potent amplifer. NIAAA data indicate a 45 % jump in CNS depression risk when any sedative is mixed with ethanol, regardless of GABA supplement use.
Even though GABA itself seems benign, the gut‑brain axis adds a gray zone. Dr. Charles O’Brien warned in 2019 that gut‑derived GABA might modulate vagal signaling, a pathway we still understand poorly. Until more data emerge, clinicians advise caution when any neuroactive supplement is added to a sedative regimen.
Practical Guidance for Patients and Providers
- Ask before you add. Over 97 % of primary‑care physicians surveyed in 2021 say they would not approve an unsupervised supplement‑sedative combo.
- Start low: 100‑200 mg of GABA, taken once daily, is enough to test tolerance.
- Avoid alcohol and other GABA‑modulating herbs while on prescription sedatives.
- Monitor with a validated scale. The Epworth Sleepiness Scale or Visual Analog Scale can flag excessive drowsiness early.
- Report any sudden drop in respiratory rate (<8 breaths/min) or blood pressure (<90 mmHg systolic) to a healthcare professional immediately.
These steps align with guidance from the American Academy of Family Physicians (2022) and patient‑focused leaflets from the Cleveland Clinic and Mayo Clinic Proceedings.
Future Directions: GABA Derivatives That Cross the BBB
Research isn't standing still. A 2023 Phase II trial (NCT04823456) is testing GABA‑C12 a fatty‑acid‑conjugated GABA molecule designed for better brain penetration. Early rodent data show a 12.7‑fold increase in CNS levels compared with plain GABA. If such compounds receive approval, the interaction profile could shift dramatically, demanding fresh safety guidelines.
Regulatory bodies like the European Medicines Agency (2022) and the FDA (2023 draft) currently classify standard GABA supplements as low‑risk for drug interactions. Clinicians should stay alert for updates as novel formulations progress.
Bottom Line
Current evidence paints a clear picture: ordinary oral GABA supplements, even at the high end of typical dosing, do not meaningfully amplify the CNS‑depressant effects of benzodiazepines, barbiturates, or alcohol. The primary safety concerns arise from other GABA‑active herbs, alcohol, or future high‑penetration GABA analogs. By keeping doses modest, avoiding additional depressants, and monitoring symptoms, most patients can use GABA supplements without jeopardizing their sedative therapy.
Frequently Asked Questions
Can I take a GABA supplement with my prescribed benzodiazepine?
For most people, the answer is yes, but only after a clinician approves it. Research shows no significant increase in sedation, but you should start with a low dose and watch for extra drowsiness.
Will GABA supplements make me feel sleepy on their own?
The majority of users report little to no effect. Any mild calmness is usually subtle and may be a placebo response.
How does alcohol interact with GABA‑enhancing drugs?
Alcohol potentiates GABAA receptor activity, so combining it with benzodiazepines or barbiturates can dramatically increase the risk of respiratory depression and loss of consciousness. Avoid alcohol entirely while on these meds.
Are herbal supplements like valerian or kava safer than GABA?
No. Valerian, kava, and phenibut actually boost GABA signaling more aggressively than plain GABA and have been shown to increase sedation when mixed with prescription sedatives.
What should I do if I notice excessive drowsiness?
Stop the supplement immediately, avoid driving, and contact your healthcare provider. Use a sleepiness scale to quantify the effect and let your doctor decide whether to adjust medication.



Kasey Marshall
October 26, 2025 AT 12:10GABA supplements are generally safe at low doses but they don’t cross the blood‑brain barrier efficiently so the effect is modest. When you add a benzodiazepine the risk is mostly from the prescription drug; the supplement adds little extra sedation. If you’re on a med like Xanax keep the GABA dose low or skip it entirely. Always talk to your doctor before mixing anything.
Jennyfer Collin
October 26, 2025 AT 13:33While the mainstream narrative presents GABA as a harmless over‑the‑counter aid, one must remain vigilant regarding potential undisclosed collaborations between supplement manufacturers and pharmaceutical entities. The data on oral GABA bioavailability is sparse and often concealed behind proprietary studies. Moreover, the concurrent use of benzodiazepines could amplify central nervous system depression beyond the intended therapeutic window. Patients should demand transparent evidence and consult independent medical professionals before combining such agents.
Tim Waghorn
October 27, 2025 AT 16:46Oral γ‑aminobutyric acid (GABA) has limited capacity to traverse the blood‑brain barrier due to its polar nature and the presence of active efflux transporters. Studies employing radiolabeled GABA have demonstrated that only a small fraction reaches central synaptic clefts, resulting in modest peripheral effects such as reduced peripheral nerve excitability. Benzodiazepines, on the other hand, bind to the GABAA receptor complex at the α‑subunit, potentiating the receptor's response to endogenous GABA and increasing chloride influx, which hyperpolarizes neurons. When a benzodiazepine is present, the receptors are already primed for maximal inhibitory signaling, leaving little room for additional modulation by exogenous GABA. Clinical evidence shows that co‑administration does not significantly alter the pharmacodynamic profile of most short‑acting benzodiazepines, but caution is warranted with high‑dose or multiple CNS depressants. Additive effects become more probable when other sedatives, such as alcohol, antihistamines, or opioids, are introduced concurrently. The primary safety concern, therefore, is not the GABA supplement per se, but the cumulative burden on the central nervous system. Patients with compromised respiratory function, hepatic impairment, or a history of substance misuse are particularly vulnerable to synergistic depression. Monitoring for signs of excessive sedation-such as slurred speech, delayed reaction time, or respiratory slowing-is essential. If any of these symptoms arise, the supplement should be discontinued immediately and medical advice sought. In practice, many clinicians advise patients to avoid over‑the‑counter GABA while on prescription sedatives, emphasizing that the marginal benefit does not justify the theoretical risk. Finally, because supplement quality control varies, patients should select products that have undergone third‑party testing for purity and potency. By adhering to these guidelines, one can mitigate the risk of unintended CNS depression while benefiting from any potential anxiolytic effects of GABA.
Brady Johnson
October 27, 2025 AT 17:36Wow, you think it’s that simple? The reality is a nightmare of compounded sedation that can turn a quiet night into a dangerous tumble into unconsciousness. Imagine the brain’s receptors already soaked in benzodiazepine, then you pour GABA on top-like adding gasoline to a fire. The result isn’t just ‘a little more relaxed’; it’s a precarious slide toward respiratory compromise. And let’s not ignore the fact that supplement labels often hide filler ingredients that can interact in unpredictable ways. If you value your safety, treat this mix with the respect you’d give any potent medication.
Jay Campbell
October 28, 2025 AT 12:13I’d just stick to the prescription and skip the supplement.
Laura Hibbard
October 28, 2025 AT 12:46Oh sure, because the best way to feel relaxed is to gamble with your brain chemistry, right?
Rachel Zack
October 29, 2025 AT 02:06People need to stop playing roulettes with their health. Taking unproven supplements while on sedatives is just reckless and irrespnsible. The moral of the story is simple: don’t mix unknowns with powerful drugs.
Lori Brown
October 29, 2025 AT 02:56You’re right, safety first! 😊 Let’s keep the conversation friendly and share reliable sources.
Jacqui Bryant
October 29, 2025 AT 03:46I think the key is to ask a doctor and follow their advice.